Pioneering Neurosurgeon - Kato Yoko
Dr. Kato Yoko is an expert in the treatment of deadly strokes, with over 3,000 surgeries to her name across a career spanning almost five decades. She also trains med students from around the world.



Transcript
FRONTRUNNERS
We've successfully isolated the aneurysm.
You do worry about causing a rupture. That would mean major bleeding.
She's a world-renowned neurosurgeon.
Very precise moves. Precise, straight.
I have to trust Dr. Kato. It's my second chance at life.
We all want to lead healthy lives.
And when an illness is found, a doctor's job is to cure it.
Pioneering neurosurgeon
Kato Yoko
Nagoya, Aichi Prefecture.
This local hospital is renowned for its world-leading neurosurgery department.
The waiting room is packed with patients from across Japan.
Thank you so much.
Many are here to see pioneering neurosurgeon, Dr. Kato Yoko.
They include 57-year-old Hattori Kazuhiro,
whose regular hospital detected some irregularities
during a recent health check.
Here they are. Blown up like balloons.
A scan revealed two aneurysms, swellings in the blood vessels of his brain.
They'll probably grow, right?
It's a bit like a volcano. There's always a risk one could rupture.
These balloon-like aneurysms are caused by a thinning of the blood vessel wall.
While both genetics and lifestyle are thought to play a part,
another key factor is age.
In some cases, the wall is so thin
that even normal blood flow can cause a rupture
known as a subarachnoid hemorrhage,
fatal in 50% of cases.
For Hattori, Kato decides on a procedure
in which small titanium clips are placed at the neck of the aneurysm
to cut off the blood flow.
His operation is scheduled for two weeks later.
You don't want that risk hanging over you.
Not when you should have 30 years left!
My father had a stroke.
So I think there may be a congenital weakness
in the blood vessels of our brains.
So if my case was left alone, I may have ended up the same way he did.
Two weeks later.
And Hattori's operation is underway.
The painstaking procedure begins with Kato's assistant, Dr. Tanaka Riki,
opening a hole in Hattori's skull to locate his aneurysms.
The next step is the clipping procedure itself.
We're waiting for you in theater two.
Dr. Kato hurries to the theater.
How's it going so far?
She works with the aid of a surgical microscope.
Deep within Hattori's brain,
the second, five-millimeter aneurysm is located at an arterial junction.
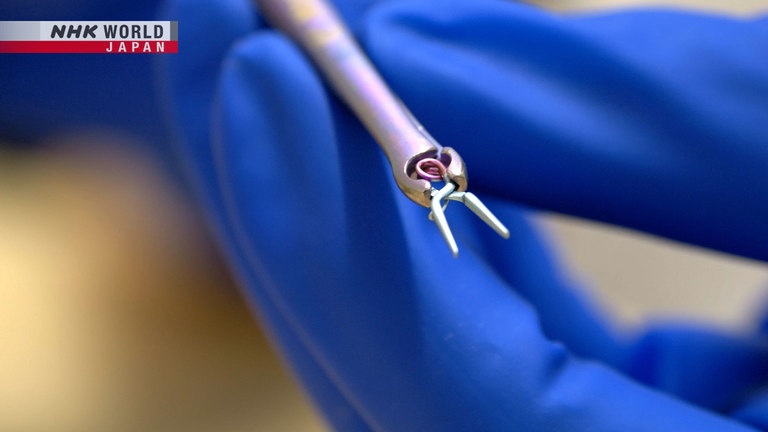
Dr. Kato uses forceps to affix an eight-millimeter titanium clip
in order to cut off the blood flow at the neck of the aneurysm.
Depending on the size and location of aneurysm,
there are over 160 varieties of clip to choose from,
ranging from 5 to 40 millimeters in length,
with both straight and curved designs.
For today's procedure, Dr. Kato selects a straight clip.
But she must take care not to damage the surrounding blood vessels,
some of which are less than one millimeter in diameter.
But as she proceeds, she encounters an unexpected problem.
There's not enough room.
It does look tight.
Space is so tight
that she risks injuring the blood vessel behind the aneurysm,
which could cause permanent damage.
Together with Dr. Tanaka,
she carefully reassesses the positioning of the various blood vessels.
And once she's sure it's safe, the operation can proceed.
But with space incredibly limited.
There is absolutely no margin for error.
Carefully, she closes the clip around the neck of the aneurysm.
Endoscope, please.
The next step is to confirm that blood flow has been successfully cut off.
The blood is infused with a special dye that glows fluorescent green.
The absence of color in the aneurysm indicates the flow has been stemmed.
We've successfully isolated the aneurysm.
Is it important to check everything?
It's crucial. Life and death.
You could end up paralyzing someone.
What can I say about Dr. Kato? She's amazing.
Of course, she puts a lot of demand on her team,
but we give our all to make sure we keep up.
She's so reliable.
When a surgical clipping is required,
having her here really improves the quality of care we can offer.
An hour later, after Hattori comes round from his anesthetic,
Dr. Kato goes to check on him.
Good job today, Hattori-san.
Thank you.
Try raising your hands. Both hands. A "banzai" pose.
And down. Now flex your fingers.
He gets the all-clear.
Comprehensive aftercare is a key part of Dr. Kato's everyday routine.
All OK? Not going back to you room?
Ah, you prefer it here?
With around three clipping operations each week,
Kato's past patients number over 3,000.
Subarachnoid hemorrhage is most common among individuals in their 50s to 70s,
causing around 10,000 deaths each year among Japan's aging population.
But it's a figure that would be even higher if it wasn't for Dr. Kato.
She's 90 and 4 months.
I'm so glad to be alive. And it's all thanks to Dr. Kato.
Her skills are god tier.
These days, 90 is pretty common.
100 is an achievement, but 90 is pretty typical.
And Dr. Kato's aftercare doesn't end at the hospital bounds.
Once a year, she goes on a rehab and support trip with former patients,
providing a valuable chance to observe their day-to-day habits up close.
As physicians, I think that is the level of insight we should aim for.
Into daily routines and so on.
And on top of all that,
I think it's a positive to receive feedback from patients.
And now aged 71, Kato also has her own health to think about.
It's all a matter of small adjustments.
Milk is better than water or tea.
I feel it's more nutritious. Packed with goodness, isn't it?
Good morning.
Dr. Kato's office regularly welcomes surgeons from overseas.
Today's group of six includes visitors from India and Bangladesh.
They're all here to receive leading edge insights into surgical clipping
that they will take back to their own countries.
Dr. Kato has spent the last three decades
proactively sharing her knowhow with medics from emerging nations.
Congolese neurosurgeon Dr. Kantenga Dieu Merci Kabulo
is nearing the end of a two-month research trip to Japan.
So, this is a clip holder and also the clips.
And as a parting gift,
Kato presents him with a set of surgical clip holders.
Dr. Kabulo is one of only 19 qualified neurosurgeons
in a country of 100 million people.
Thank you professors, thank you everyone.
And he intends to put the lessons learned here into practice
with the first-ever clipping procedures in the Democratic Republic of Congo.
These, we aren't going to keep them, we're going to use them.
And after we've used them, we'll send you the pictures that you will see.
And don't get tired of us if every time we ask you for advice from your side.
Thank you so much.
I think he's a great example.
You can be the leader of the African countries. Definitely.
And as Dr. Kabulo returns home,
the hospital welcomes two more neurosurgeons from war-torn Ukraine.
My name is Andriy. Surname, Dyakiv.
I come from Ukraine.
Hello everybody, nice to meet you all.
My name is Yuriy, my surname is Flys.
Both hail from the same hospital in Lviv, in the west of the country.
As I said, now we have a lot of military patients
from the east side of Ukraine.
So from the site, they're transferred by plane?
By train.
By train?
By train, yes.
That is a train prepared for the military, with all equipment.
They are transferred on a bed.
They can treat even in the train?
Yes. Not surgery, but yes.
Amidst a conflict, their neurosurgical expertise is especially precious.
And mindful of a constant need to improve their skills even in times of crisis,
they are here to observe Dr. Kato's clipping procedures in person.
You want to come here? Please.
How to place the clip, so that is another problem.
It is very complicated.
So, but, no need to place only one clip.
You can do a combination of clips.
Or, you can divide the aneurysm because this is not ruptured.
She does very quick clipping.
And 100%, she understands what she's doing.
It was very nice to see a surgery like this.
And very precise moves. Precise, straight. Very good.
And as well as welcoming visitors to Nagoya,
Dr. Kato has traveled at her own expense to pass on her skills
to medics in over 40 countries and regions around the world.
In 2021, these tireless efforts earned her a Lifetime Recognition Award
from the American Association of Neurological Surgeons.
In November, as President of the Asian Congress of Neurological Surgeons,
she hosted a webinar for colleagues in Africa.
Joined by Dr. Kabulo, who, just two months since his return,
has already put her lessons about clipping into practice.
I came back to Congo, and in Congo,
I did my first clip which was the first one clipped
by a permanent Congolese neurosurgeon.
And this was day two, post-op.
The patient could talk, could stand, and walk.
Thank you so much, and thank you again to Professor Kato for training us.
Thank you.
I congratulate you for your achievement.
It must've been quite difficult because it's such a huge edema.
I'm very pleased.
Two thirds of countries across the African continent still lack neurosurgeons.
But if we can establish several leaders there,
they can spread that expertise.
That's what we're trying to do.
Dr. Kato's medical roots go back to her father.
Also a surgeon, he founded this small hospital in northern Nagoya.
And Kato still returns every Saturday to provide care for local people.
Your scan is all clear.
Thank you, doctor.
Your brain looks fine.
She's the local grocer.
Keep working - that'll keep you fit. And come again whenever.
Kato Yoko was born in 1952,
to heart surgeon Koichi and school teacher Hisae.
And Koichi too placed great emphasis on patient care.
He'd keep a close eye on patients, and listen to them carefully,
even about little things,
about their family and so on.
He took all that in.
Younger brother Hajime also went into the medical profession,
taking over the family practice.
It was the natural path for both siblings to take.
Nobody ever told us to choose this direction.
It just happened naturally.
Yes, that's right.
I wasn't cut out to be a teacher like our mum.
So the only thing for it was to follow after dad.
I suppose back then I did use to
find the constant back and forth of ambulances rather exciting.
In fact, she still lives on the third floor of this hospital.
After her father died, she stayed here with her mother.
Until Hisae too passed away last year at the age of 96.
One thing about living alone is the lack of chances to talk out loud,
about little daily choices and so on.
Sometimes, I talk to mum's picture on the altar.
I mean, I wasn't the best daughter.
We didn't use to go on trips or to hot springs together.
It was Kato's dynamism and energy
that saw her med school professor recommend neurosurgery.
And at the age of 39, she began her career as a surgeon.
But in those days, some patients had an aversion to female doctors,
while senior male colleagues who saw her as a hindrance
would even exclude her from the operating room.
But she found solace and inspiration
in her mother's successful balance of family life and her career in education.
Whenever I used to grumble about my troubles,
she'd always just say "What's up with you?"
No advice, but she helped me put things in perspective.
That's how she was, very... "matter-of-fact" you might say.
Now, 40 years into her career,
Dr. Kato's fame as a neurosurgeon stretches far beyond the borders of Japan.
But even today, she sometimes encounters patients
who present totally new challenges.
Like 66-year-old Kabeya Nobuko.
After a lifetime of good health,
she was referred to Kato after a scan revealed a brain aneurysm.
Hello. Are you her daughter?
Your mom was referred to me with an aneurysm.
But structurally it's rather unusual.
Here we see some arteriosclerosis.
The yellow here denotes arteriosclerosis, a hardening of the artery walls,
including the area of the aneurysm itself.
Non-invasive treatment would be tough.
After a lot of consideration, I think we need to go in for a closer look.
Unable to decide the right treatment from a scan alone,
Kato recommends an exploratory craniotomy.
Does this procedure carry any risk of lasting complications?
The worst possible outcome could be paralysis down her right side.
But we'll work to avoid that.
Kabeya's case carries a lot of uncertainties.
Want to speak to another recent patient?
I'll call her in.
You're about the same age.
Dr. Kato calls for another patient
who underwent a craniotomy several days ago.
The aim is to calm Kabeya's worries about her own procedure.
It's helped ease my fears.
I have to trust Dr. Kato, as I can't fix this myself.
So I've decided to leave it to her.
The day of Kabeya's operation arrives.
How does it look? Rock solid?
Yup. With some little red speckles.
The hardening of the artery
rules out affixing a clip at the neck of the aneurysm.
Wow. It is rock hard.
This is the only bit I can get hold of.
But while the area is too stiff to pinch off,
this small red patch denotes a thinning of the wall.
A rupture here could be fatal.
Dr. Kato decides the only choice is to clip this area.
The slightest mistake could be disastrous.
They double check for other nearby risks.
This bit's really hard. Just like it's turned to stone.
Wait, is this another aneurysm?
Let's clip that too.
They detect another small patch with a risk of rupture.
I'm going to divide this into two.
Dr. Kato decides to clip both locations.
First, she places a straight clip.
Then, she uses an angled clip to cut off the second delicate patch to the left.
The clips are in place.
Are we good?
The challenging operation takes twice as long as a standard procedure.
The wall of these aneurysms was very thin,
so I was worried they might rupture when I placed the clips.
That would have caused major bleeding,
so much so that I wondered how to proceed.
It was crucial to ascertain which spots were safe and which weren't.
But I think we managed to isolate the danger.
A month later, we find Kabeya playing with her granddaughter.
Last week, we played together all day.
If it hadn't been caught,
I really could have died at any moment.
I'm so lucky we identified the risk.
Keep your chin up through today's rehab.
After you.
So what is it that continues to motivate Dr. Kato Yoko
as a "frontrunner" in her field?
At the end of the day, most people look to doctors for diagnosis and cure,
and that's what I want to provide.
That's the motivation that keeps me going.