ICIs: Key to Surviving Cancer
While immune checkpoint inhibitors can improve cancer survival rates, they only work in about 20 to 30% of patients. We interview Japanese researchers who are trying to overcome this challenge.
Transcript
Cancer, once seen as challenging to treat, has become a manageable disease
thanks to significant advances in medical technology.
Immune checkpoint inhibitors have played a key role in this transformation.
Immune checkpoint inhibitors, or ICIs, are drugs that help maintain the immune system's ability to fight cancer.
ICIs, a type of immunotherapy, have gained attention as the "fourth cancer treatment"
after surgery, chemotherapy and radiotherapy.
In 2018, Honjo Tasuku won the Nobel Prize in Physiology or Medicine.
His discovery contributed to the development of ICIs.
ICIs can nearly eliminate cancer, even when it has progressed and spread to other organs.
They have successfully extended patients' lives.
In Japan, seven types of ICIs have been approved as of mid-2024.
They are used to treat over 10 types of cancer, including lung, stomach, breast and colorectal cancer.
While immune checkpoint inhibitors can have dramatic effects for some cases of stage 4 cancer,
they only work for about 20 to 30 percent of all patients with the disease.
We'll explore the forefront of Japanese research that aims to overcome this challenge
and to make immune checkpoint inhibitors accessible to more people.
10 years have passed since cancer treatment with ICIs began in Japan, ahead of the rest of the world.
Lung-cancer patient Miki Masahiro decided to undergo this treatment.
In 2015, cancer was found in both of his lungs.
He received a diagnosis of stage 2B.
Despite chemotherapy and radiotherapy, the cancer returned and spread to his brain.
In 2017, the cancer recurred a second time in his left lung.
His doctor suggested treatment with ICIs.
I'd heard that immune checkpoint inhibitors were quite effective for some people.
So I decided to try them.
You won't know if a therapy will work until you try it.
I just wanted to give it a shot.
Miki began the treatment, receiving an ICI via an intravenous drip every three weeks.
Two and a half months later, significant changes began to appear.
My doctor said, "It's working dramatically."
I was surprised by his enthusiasm.
The cancer, which had been about the size of a fingertip, had shrunk to just a few millimeters.
I thought, "Wow, it's really working." I was amazed.
Our immune system detects and attacks pathogens and other foreign objects that enter the body.
It also targets cancer cells, which develop due to abnormalities in normal cells.
This footage shows a cancer cell being killed by a type of immune cell called a T cell.
Cancer cells form in our body every day.
But our immune system, centered around T cells, continuously kills them, preventing the development of cancer.
T cells are the key to understanding how ICIs work.
Some cancer cells manage to survive.
They do this by stopping T cell attacks.
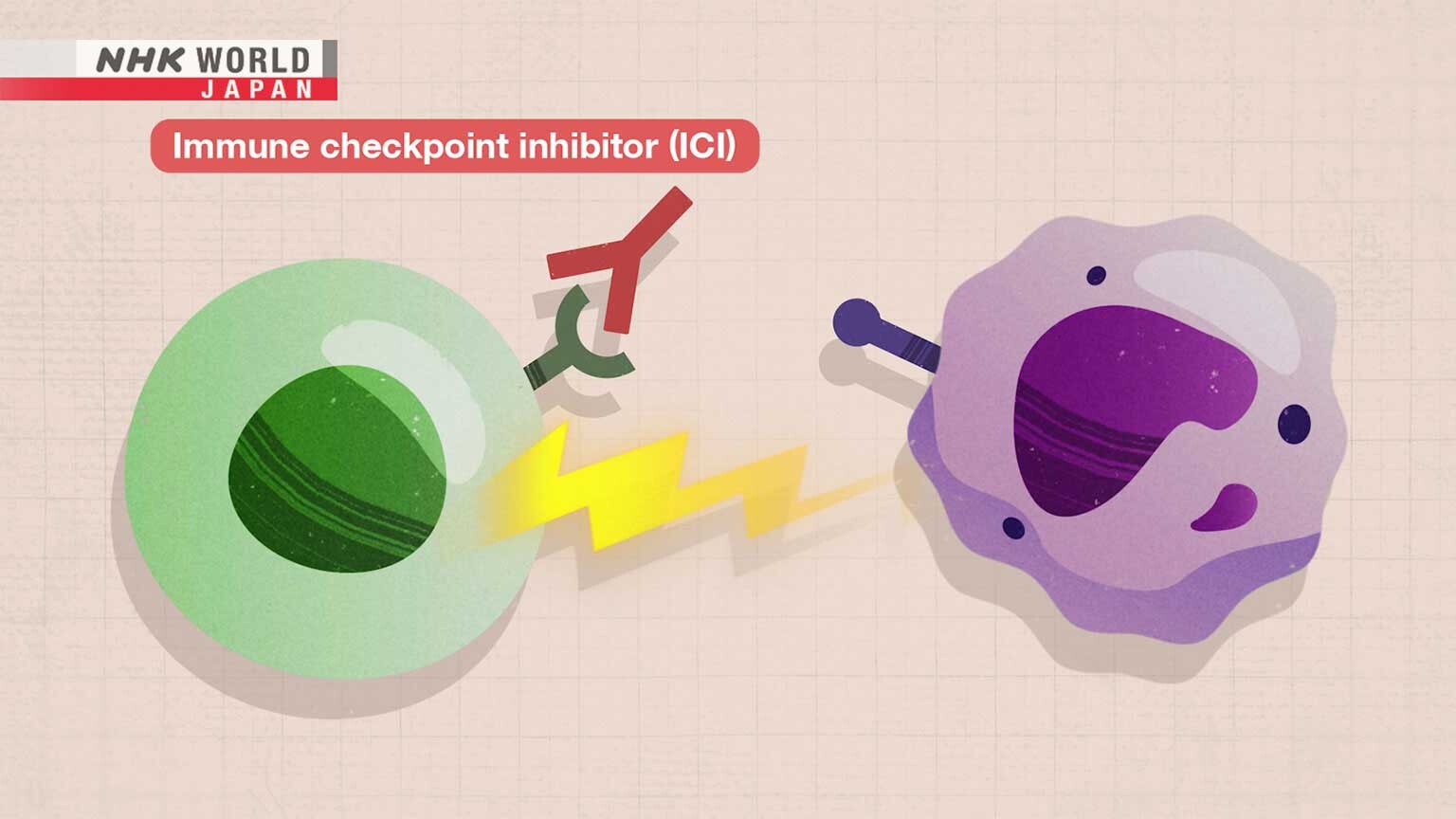
T cells have brakes on their surface to stop them from launching excessive attacks that could damage healthy cells.
One such brake is the PD-1 molecule.
To activate this brake, cancer cells produce a molecule called PD-L1.
When PD-L1 binds to PD-1 on T cells, the brake is applied, stopping the attack.
This mechanism is known as an immune checkpoint.
ICIs block this immune checkpoint, allowing T cells to resume their attack.
By preventing T cells and cancer cells from binding, ICIs stop the brake from being applied.
T cells can then keep attacking and killing cancer cells.
To learn more about ICIs, we spoke with lung-cancer expert Seike Masahiro,
who is involved in an international clinical trial for these drugs.
I believe we can say that treatment has shifted fundamentally.
The way we think about drug therapy for lung cancer has undergone a dramatic change.
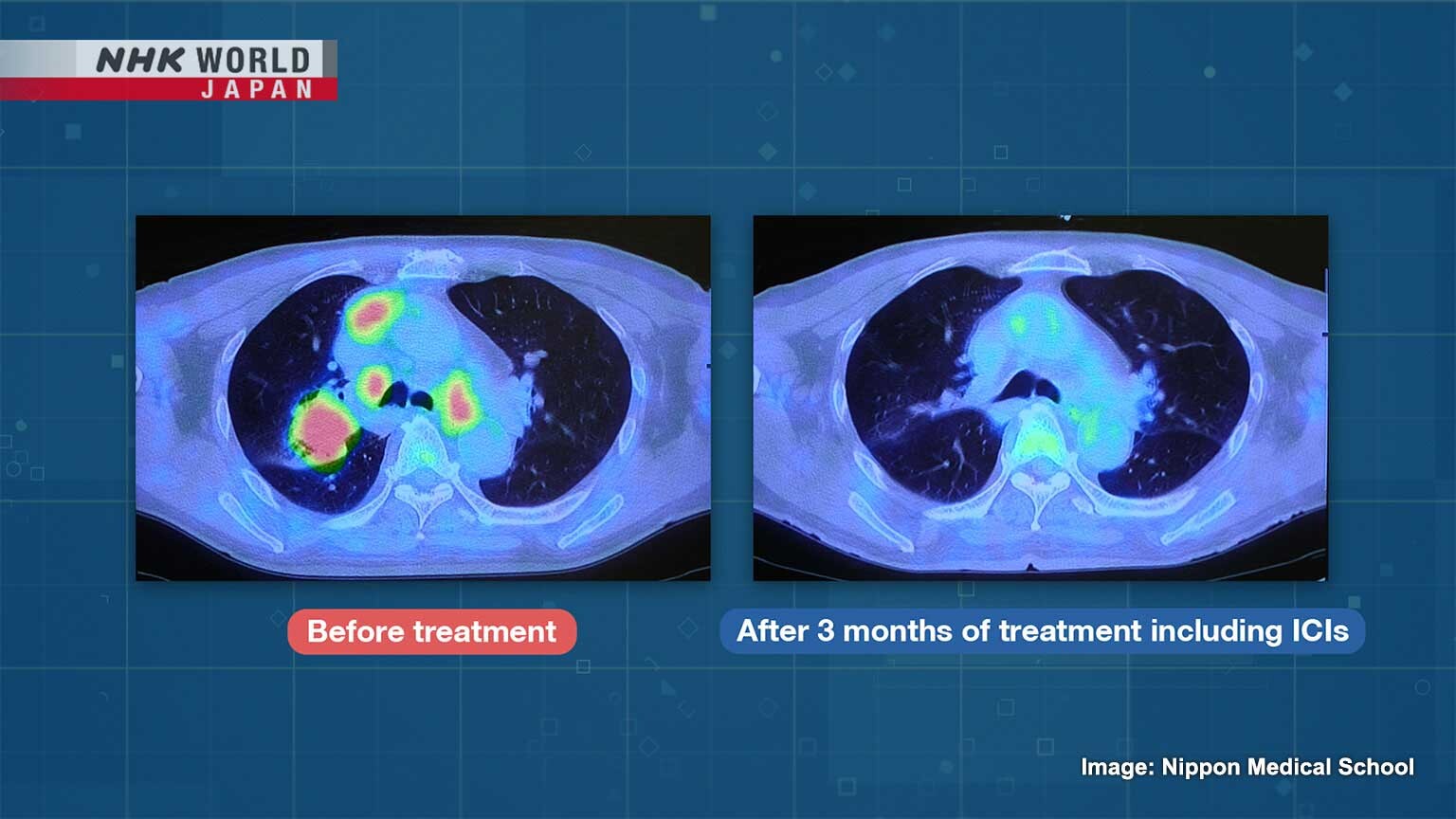
This is a PET-CT scan image of the lungs of a stage-4 lung-cancer patient.
The cancerous parts are shown in red.
The primary lung cancer measures about four centimeters.
It has spread to nearby lymph nodes.
The cancer had also spread to the bones.
The patient first came to us in a wheelchair, unable to walk due to severe lower back pain.
Seike suggested a treatment using both anticancer drugs and ICIs.
Three months after starting the combined treatment...
the cancer had almost disappeared.
One year after discontinuing the medication, the patient is healthy enough to visit the hospital on foot.
It takes some time for ICIs to work.
Anticancer drugs will buy us some time until the ICIs start working.
This is a graph comparing the survival rates of stage 4 lung-cancer patients treated with chemotherapy alone
and those given a combination of chemotherapy and an ICI.
The five-year survival rate for chemotherapy was only 11.3 percent.
When combined with an ICI, it was 19.4 percent.
Patients with advanced cancer are surviving for 5 years or even being cured.
Immune checkpoint inhibitors have introduced a new era in which lung cancer can be cured.
However, ICIs can overly activate the immune system, causing side effects
such as colitis, thyroid dysfunction, interstitial lung disease and dermatitis.
Miki did not experience any side effects.
He completed his treatment and has regular checkups.
Three years after he stopped taking medication, he remains cancer-free.
Miki used to be a chef of Chinese cuisine.
He now spends his days quietly and enjoys making pork buns in his garage.
Having had lung cancer, I'm grateful to be in this condition even almost 10 years later.
I'm glad to have something to do, like making pork buns.
Sharing his home-made pork buns with family and friends brings him great happiness.
It's delicious!
ICI treatment involves a significant challenge.
These drugs are effective for only 20 to 30 percent of patients,
and it is difficult to accurately predict who will respond until the treatment is tried.
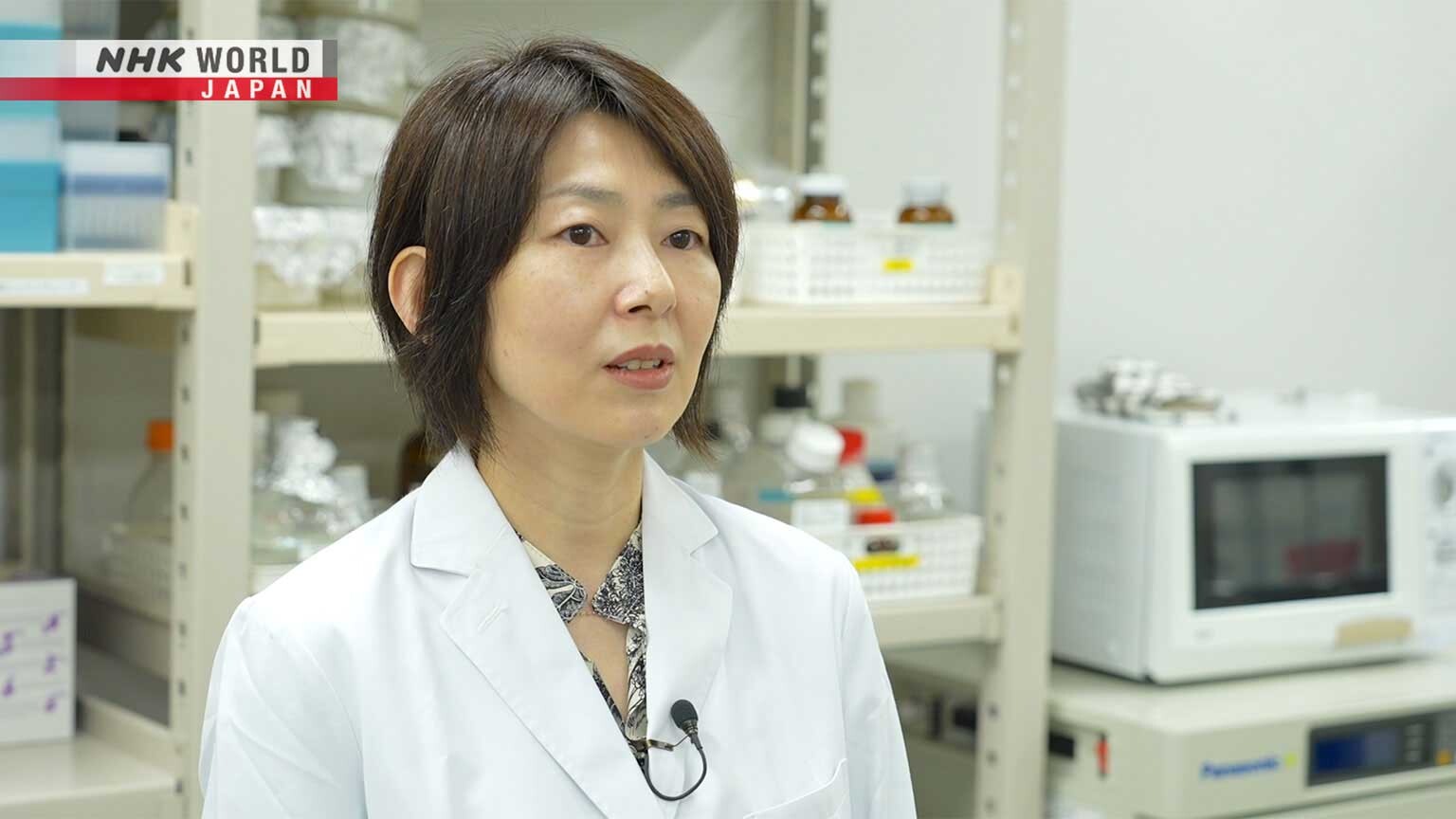
Iwai Yoshiko is trying to uncover the reasons for this.
She aims to establish a method to determine who will benefit from ICIs.
Iwai made a major contribution to the development of ICIs as a member of Nobel laureate Honjo's research team.
She was involved in finding PD-L1, which puts the brake on T cells.
She also helped to create an antibody to prevent this braking.
Immune checkpoint inhibitors or ICIs are proving increasingly effective for different types,
particularly for advanced cancers.
So what are your thoughts on this?
ICIs offer a new option for patients who could not be cured with other therapies.
I am very pleased as both a physician and a researcher.
What sort of research are you currently working on?
We're trying to make a test using blood to tell who will benefit from ICIs and who won't.
Iwai began this research after examining a graph comparing the changes in survival rates for ICIs and chemotherapy.
What caught Iwai's attention was the ICIs' L-shaped curve.
After a sharp decline in the survival rate, it stabilizes.
This suggests that ICIs are effective for some people, but not for others.
Iwai believed that by uncovering the reasons for this,
it would become possible to accurately predict who will respond to ICIs.
As a developer of ICIs, I want them delivered safely to the right patients.
They're currently administered to patients even when it's unclear whether they'll work or not.
This really concerns me.
If we could avoid giving them to patients who may not benefit, ICIs would help more people.
Using blood samples from non-small cell lung cancer and gastric cancer patients,
Iwai discovered two important markers that determine ICI effectiveness.
She co-authored a research paper published in 2024 in a leading international pharmacology journal.
The first marker measures the strength of the body's immune response.
The immune response is the action taken by immune cells against foreign substances.
A strong response attracts many T cells to cancer cells.
The cancer cells secrete PD-L1 to stop T-cell attacks.
Only then does the ICI become effective, halting this mechanism.
However, if the immune response is weak, fewer T cells gather around the cancer.
As a result, the cancer cells will be less likely to release PD-L1 to stop attacks.
Even if an ICI is taken, its effectiveness will be limited.
In fact, parts of the PD-L1 secreted by cancer cells enter the bloodstream.
Iwai discovered that by measuring the amount in the blood,
the strength of the immune response can be determined.
The second marker indicates whether blood vessel walls break easily.
Some people have fragile blood vessel walls that are easily damaged.
Cancer cells can enter the bloodstream through the broken walls and spread to other parts of the body.
Considering only the immune response is not enough to assess a tumor.
We must look at malignancy and damage to blood vessel walls to determine treatability.
That's our new finding.
In an experiment, Iwai divided patients into three groups based on blood-sample data and analyzed their survival rates.
The results showed that ICIs were most effective for the group with strong immune responses and durable blood vessel walls.
These patients had a survival rate of about 80 percent.
Those with weak immune responses also benefitted to some extent, with a survival rate of 40 percent.
But the group with strong immune responses and fragile blood vessel walls experienced a rapid decline,
with many passing away in about one year.
As a patient, knowing early on in treatment whether a method is suited to you is helpful.
It will allow both you and the doctor to figure out the best course of treatment.
That's the biggest advantage.
Iwai is working with a testing company, aiming for practical application within 3 years.
We're not done yet. We would like to pursue further.
We're hoping to come up with a treatment for people for whom ICIs are not effective.
That's our current goal.
ICIs are only effective in about 20 to 30 percent of patients.
Researchers worldwide are now looking into a promising solution to this challenge: intestinal bacteria.
Takeda Kazuyoshi has been studying the relationship between cancer and intestinal bacteria for almost 30 years.
The intestines are crucial for digesting food and absorbing nutrients.
They're also home to many immune cells.
Intestinal bacteria are closely linked to immune cells.
Researchers are hoping that these bacteria will boost the effectiveness of ICIs.
In 2022, Takeda and his research team found through mouse experiments
that a substance produced by a certain type of lactic acid bacterium increases the effects of ICIs.
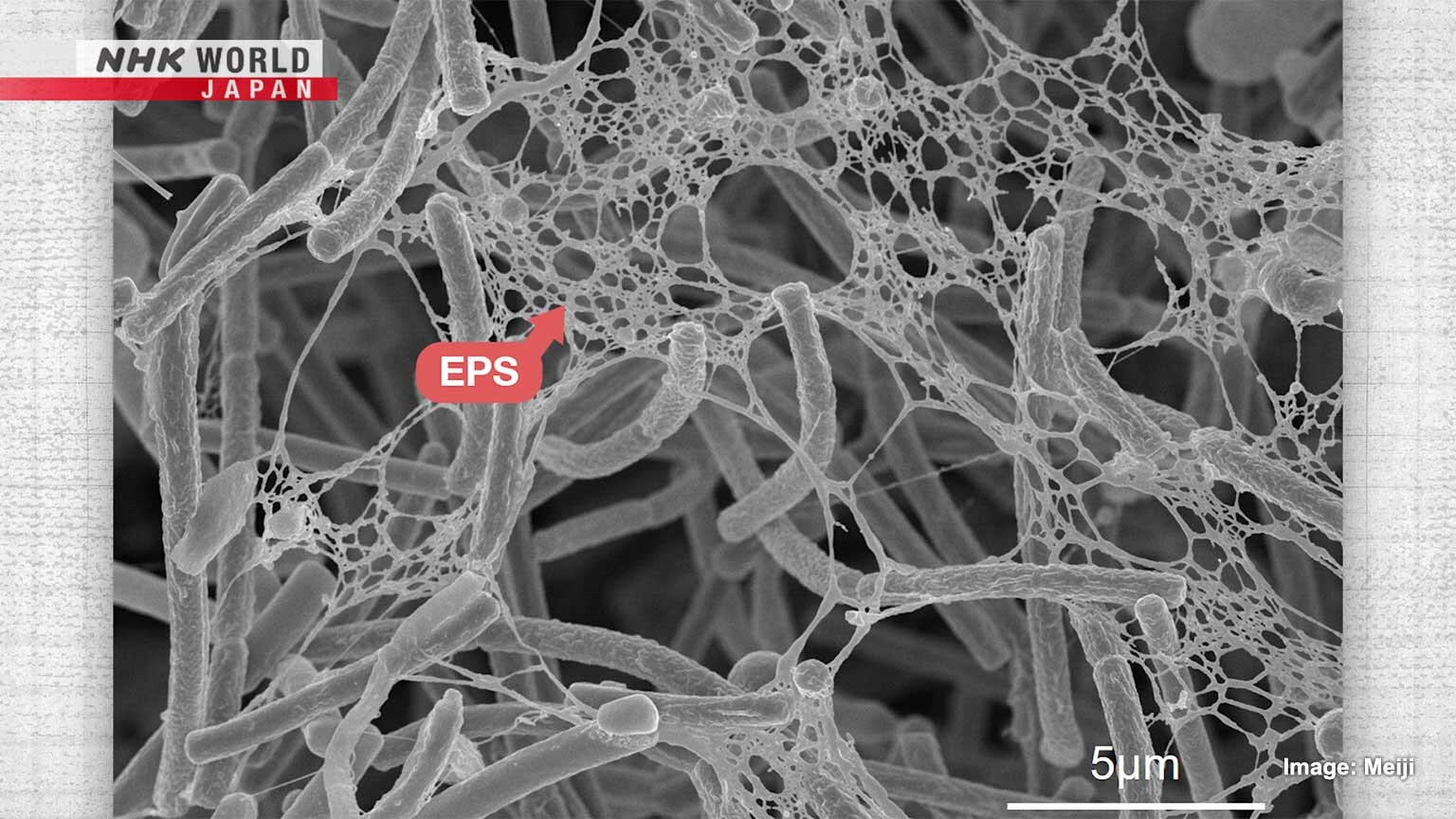
I found that EPS, a lactobacillus-made polysaccharide, boosted the effects of ICIs.
This image shows EPS, the mesh-like structures stretching from the rod-shaped lactic acid bacteria.
When EPS is absorbed into the intestines, it stimulates the T cells there.
These stimulated T cells travel through the body and find cancer cells.
They then attract attack-oriented T cells.
EPS doesn't attack cancer directly. EPS-activated T cells don't, either.
T cells are activated by EPS in the gut and travel to where the cancer is.
There, they support the T cells that do the attacking.
Experts think that people who don't respond well to ICIs
have weak immune responses and few T cells around the cancer.
Takeda believes that when T cells are stimulated by EPS,
they attract attack-oriented T cells to the cancer, creating an environment where ICIs are effective.
EPS-activated T cells are game-changers. What was once a disadvantage can now be altered.
They can boost immune responses.
Takeda gave two kinds of ICIs to mice transplanted with cancer cells.
Some mice received only an ICI, while the others were given oral EPS alongside the ICI.
These tumors were taken from each mouse 15 days after the experiment.
Those in the top rows came from ICI-only mice.
Below are from the ICI-EPS mice.
There was more tumor shrinkage in the latter group.
These graphs show changes in tumor size.
The red lines represent the ICI-only groups,
while the blue lines show the groups that received an ICI and EPS.
In both cases, the mice that were also given EPS had slower tumor growth rates.
Mouse experiments have shown that combining ICIs and EPS is effective in treating colorectal and breast cancer.
The research team is considering how this could be applied to humans, including the development of medications.
When Takeda began his research, the idea of treating cancer with the immune system was met with skepticism worldwide.
But ICIs have drastically changed the research landscape.
Originally, research on using the immune system to fight cancer constantly faced setbacks.
With ICIs, we're finally winning and aim to keep winning. There's still room to improve.
We want to expand the potential of treating cancer with the immune system.
Today, acupuncture and moxibustion practitioner, Edward Obaidey,
will share some tips for maintaining a healthy body.
Obaidey came to Japan in 1987, where he studied acupuncture and moxibustion.
He obtained a national qualification and opened a clinic in Tokyo.
If we look at the traditional way of looking at it,
looking at it from the viewpoint of Ki, we need Ki to function.
Also, we need Ki to protect ourselves.
Without ki it's a bit like having a car without the electrical system,
without the gasoline to move it.
In Eastern medicine, "Ki" refers to the energy necessary for life.
Enhancing the energy in organs like the kidneys and the lungs is believed to lead to overall well-being.
The first tip aims to boost kidney energy.
We'll do a few easy exercises that make up one set.
Let's begin with a simple breathing technique.
It's just taking the energy that's normally up here, which we will have and it is putting it down there.
And if we put it down there, it will help the kidneys.
Does that mean the energy is kind of stuck up here?
Yeah. So we have a simple movement where we just use the body to take the energy up
and then let it down.
Stand straight with your feet shoulder-width apart, palms facing upward,
and raise your arms as you inhale.
When your arms are near your head, bend your elbows, palms facing down, and lower your arms slowly as you exhale.
Try not to arch your back too much.
Repeat this 15 times.
Obaidey says this improves blood circulation and prepares your body to be filled with energy.
Next, let's move the shoulders.
Slowly rotate each shoulder in a large circle, one at a time, to further enhance the flow of energy.
This requires a sort of lazy effort.
- And I like the emphasis on lazy.
- Lazy, lazy.
Obaidey says it's important not to use too much force.
Relax and repeat it 30 times.
For the third exercise, we'll use a split bamboo, a health tool long used by the Japanese.
In Eastern medicine, stimulating the entire sole of the foot is thought to increase the energy in the kidneys.
Start with one foot, then try both after getting used to it.
Do this for around three minutes.
It's quite interesting. This sensations are very different in different parts of the foot.
- Yes.
- I mean, I would imagine this lots of different benefits.
But if you were to describe some of the main benefits, what would they be?
I would say number one, it starts to turn this off.
It brings the Ki down from the head, takes it away from our overworked mind.
And the other thing is, after this, you probably sleep better.
You can also use a golf ball instead of bamboo.
Roll it under your feet.
Finally, repeat the first breathing exercise we did five times.
Relax, and it's done.
Next, we'll focus on energizing the lungs.
In Eastern medicine, increasing the energy in this part of the body is believed to prevent colds.
Warm the acupoints behind the neck and upper back.
Use a hair dryer while massaging softly.
Be careful not to burn yourself.
Great. Because I think everybody can kind of reach over the hairdryer and do it themselves,
will get their partner do it if they live with someone.
Now for people that are sweating a lot, maybe the beginning of a cold.
You do this very gently with a little bit further away,
and you rub and you do this until the sweating stops and then that's enough.
Obaidey says warming the back of the neck with a hot towel or a hot-water bottle is also effective.
I think the key point is not pushing yourself too much.
Yeah, I think especially in the West, we can learn from the East,
about being a little bit more, less radical,
I should say, with the way that we exercise and the way we think about health.
So you should be lazy effort.
So Edward, thank you so much.
Thank you. It's been a pleasure talking to you, I tell you.