Preventing Blindness With iPS Cells
iPS cells are being used to treat eye diseases to address donor shortages. We explore advancements made in Japan, such as the transplantation of iPS cell-derived corneal cells and retinal sheets.



Transcript
In Japan, efforts are now underway to prevent eye diseases that can lead to blindness if left untreated.
This involves a new stem cell therapy that uses genetically reprogrammed stem cells called iPS cells.
Professor Shinya Yamanaka was awarded the Nobel Prize in 2012 for his development of iPS cells,
and since then, clinical trials involving patients have been progressing rapidly in Japan.
Today, we're going to bring you the latest on iPS cell therapy aimed at preventing blindness.
The human body begins with just one cell: a fertilized egg.
The cell divides and multiplies, eventually ifferentiating into various parts of the body with specific roles.
Creating induced pluripotent stem cells, or iPS cells,
is like artificially turning back the cellular clock to a state similar to a fertilized egg.
Specific genes are introduced into human cells to turn them into iPS cells.
Like fertilized eggs, iPS cells can develop into any tissue or organ in the human body, including the heart, nerves and blood.
In Japan, researchers have been using iPS cells in clinical trials on people with heart disease,
spinal cord injuries and Parkinson's disease.
In 2022, Keio University performed the world's first transplant of iPS cell-derived cells for the innermost surface of the cornea.
The eye is a sense organ that takes in light.
At the front is a clear layer that protects the eye.
It's called the cornea.
Light passes through the cornea, stimulates the retina, then travels via the optic nerve to the brain.
If the cornea is damaged and cannot heal with medication,
the only treatment option is to transplant a cornea from a donor.
This woman had a condition called bullous keratopathy.
She had a traditional corneal transplant from a donor overseas.
Bullous keratopathy occurs when the corneal endothelial cells in the innermost layer of the cornea are damaged,
causing fluid to build up in the cornea.
As a result, the cornea becomes thicker, swollen and cloudy, and vision worsens.
If left untreated, it can lead to blindness.
I would have intense pain, and my eyes would get very bloodshot.
I'd feel stinging and a dull, throbbing pain.
My tears just wouldn't stop. That's what my symptoms were like at their worst.
She was anxious before undergoing the transplant.
It's impossible to know if rejection will occur until after the transplant.
Although it's less common than with other organs, it's still a possibility.
I worried that it would happen to me.
However, the transplant changed her life.
I opened my eyes and was amazed by the bright, colorful view.
I felt so relieved.
The blurriness was gone.
But not all cases are as successful as hers.
Around 13 million patients worldwide are waiting for a corneal transplant.
However, due to a shortage of donors, only about 180,000 people can have the procedure each year.
About half of the patients awaiting a transplant are believed to have bullous keratopathy.
The transplant in 2022 using iPS cells was performed on a patient with bullous keratopathy.
It was done by Shimmura Shigeto, a professor currently at Fujita Health University.
You know, Japan really is at the forefront of regenerative medicine, and it's such an incredibly exciting field.
So thank you so much for your time today.
You're welcome. My pleasure to be here.
I think one of the key issues just looking at the stats is 13 million people worldwide.
Waiting for a corneal transplant.
I mean, it's just staggering - the amount of people who are waiting for this.
So what we want to do is that instead of using donor corneas,
where in that case we need one cornea for one patient.
Instead, if we can use cultured cells, we can make enough cells.
So we've been trying to do this for over ten years.
Shimmura and his team have overcome various challenges
to make the transplantation of iPS cell-derived tissue into humans a reality.
And in terms of the potential for an iPSC cell,
there's talk in the literature occasionally about the potential for it to be cancer causing.
The regulatory procedures that we have to go through to show that these cells are safe is very strict.
So we did that.
We've done a lot of transplants in mice to show that these cells do not become tumors.
Scientists believe cancer can develop when some iPS cells don't fully differentiate
into the intended cell types during the culturing process.
By carefully controlling the culturing process,
Shimmura's team succeeded in creating iPS cells that do not become cancerous.
The team also did transplantation experiments on monkeys.
This image shows the eye of a monkey with bullous keratopathy.
It's white and cloudy.
This is a monkey's eye 28 days after iPS-derived cells were transplanted.
After the transplant, the eye is no longer cloudy and has regained its clarity.
Now, let's look at the corneas' thickness.
The corneas of the monkeys that didn't receive a transplant remained thick.
But in the monkeys that had a transplant,
corneal thickness returned almost to normal levels 28 days later.
This indicates that swelling had subsided.
After more than 10 years of conducting experiments like these,
Shimmura's team finally transplanted corneal endothelial cells derived from iPS cells into a human patient.
They used the iPS cells created from another individual, not the patient themselves.
Therefore, there were concerns that rejection would be more likely than if the patient's own cells were used.
So in a standard corneal transplant procedure, we only use eye drops to suppress immunity,
steroid eyedrops, and we use these drops for a few years.
On the other hand, we're figuring out or were you finding out now that
the less tissue that you transplant into the patients,
the less immune response we get, which is quite interesting.
Typically, in traditional donor transplants of the entire cornea,
rejection occurs in about 20 to 30 percent of patients.
But when only corneal endothelial cells are transplanted, the rejection rate drops to around 2 to 5 percent.
Therefore, Shimmura expected that transplant rejection would be less likely
with corneal endothelial cells made from iPS cells.
And in terms of the procedure itself, is it like a transplant?
Are you putting in a sheet or a lens or how is the procedure actually done?
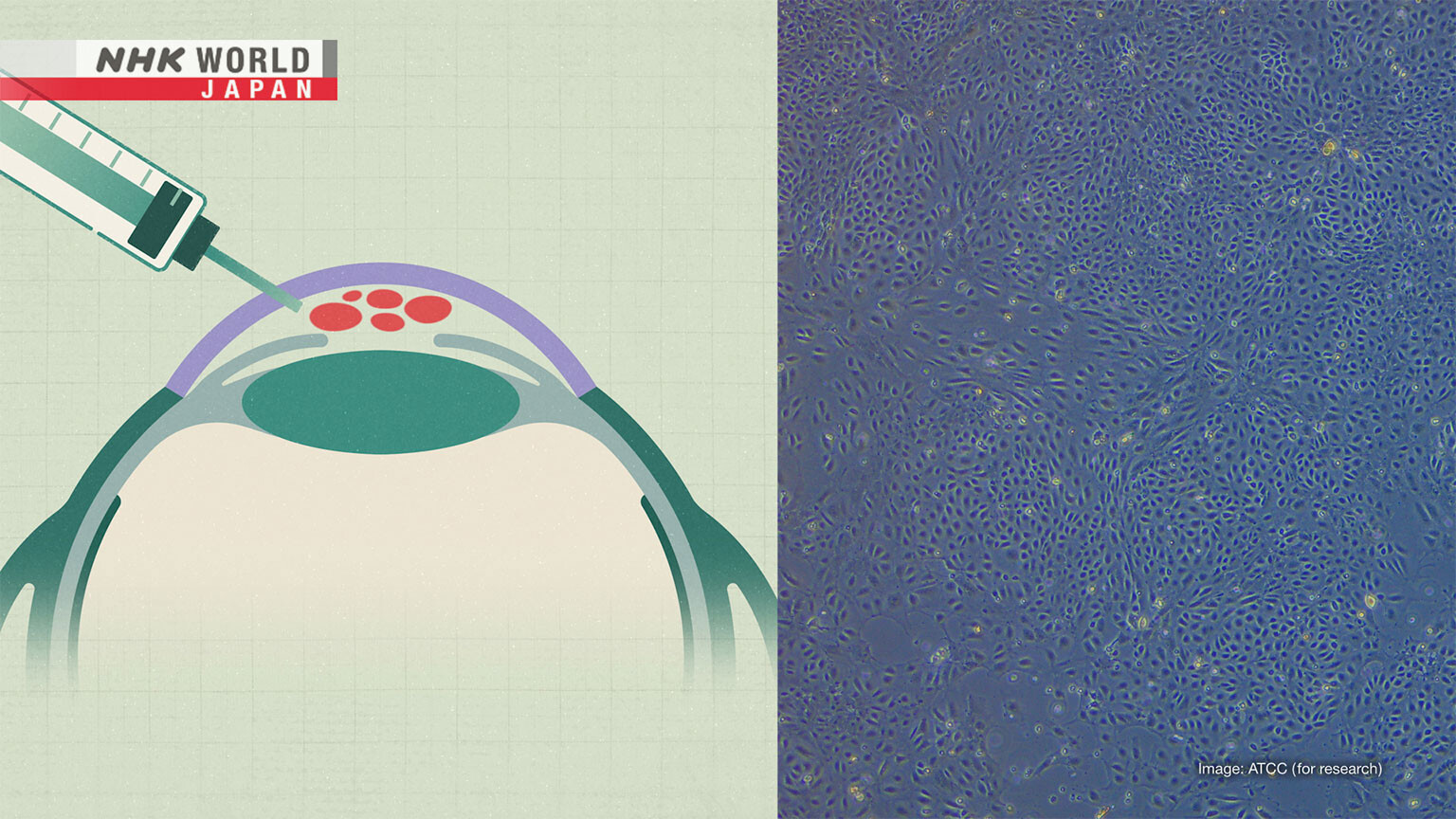
It's just an injection of cells using a syringe and we just put it into the eye.
So it's much safer, much shorter.
About 800,000 iPS cell-derived corneal endothelial cells are injected into the patient's cornea.
The procedure takes about 20 minutes.
The patient will then lie face down for about three hours to allow the cells to settle.
Traditionally, transplants of the entire cornea involve surgically sewing a donor-provided cornea in place.
The doctor must have advanced skills.
However, transplants using iPS cells are simpler and less burdensome for patients.
There are high hopes for its success.
When you first completed the first iPS cell-derived cornea transplant, how did you actually feel?
I felt relieved.
I felt relieved that nothing happened to the patient or there were no adverse effects.
So I think that cornea transplant is the next step in towards reducing the number of blind patients
due to corneal disease because most of these patients, if they get the transplant,
they can see most of the people who are blind due to corneal disease,
they have healthy retinas.
So if they can restore the clarity of the cornea, they should be able to see.
And in terms of efficacy, meaning whether these cells work,
we're going to start a larger scale trial in a couple of years.
I think that for the medicine as a whole,
it's important that people have several choices to treat whatever disease they have.
And there are several ways to treat these cells.
Corneal transplants, we cultivated donor cells,
but I think that having more options is better for the patient.
And our ultimate goal is to come up with the therapy that is scalable, safe and easy to use.
A key to promoting transplants involving iPS cells is the large-scale production and widespread availability of these cells.
A startup that conducts joint research with Shimmura
has made it possible to create large amounts of iPS cells from human sources.
These dots are individual iPS cells.
Scientists spend about three weeks culturing iPS cells.
Then, over the following two weeks,
they allow the iPS cells to differentiate into corneal endothelial cells.
How many cells - for example, when it gets to that stage of one month,
in this stage, how many cells are in there?
We start with 1 batch of iPS cells.
We can grow them to produce enough corneal endothelial cells for 1,000 patients.
I mean, the potential to help thousands and thousands of people is quite incredible.
Where when you think it's only in the scale of 1 month. Just quite a short period.
We hope that iPS cell technology can be used to treat patients worldwide.
The cells can be preserved through freezing.
The company believes this will allow the cells to be transported not only within Japan but also abroad,
making transplants possible worldwide.
We hope to commercialize these cells in Japan by around 2027, ahead of the rest of the world.
Our mission is to provide treatment using these cells to patients globally.
We aim to make our cells available around the world by around 2030.
Clinical research is also being done on the use of iPS cells for the retina, at the back of the eye.
In 2014, the Kobe City Eye Hospital became the first facility in the world to start retinal transplants using iPS cells.
So far, it has performed the procedure on 10 patients with severe conditions.
These transplants prevented what was considered an unavoidable decline in their eyesight.
None of the patients experienced serious side effects.
Since 2020, the hospital has been at the forefront of global efforts in using iPS cells to treat retinitis pigmentosa.
This is an intractable disease that occurs when the cells in the retina are damaged.
The number of light-sensitive photoreceptor cells decrease, and vision gradually declines.
There's no treatment yet that can lead to recovery.
Because the retina loses function upon a person's passing, transplants from donors are not possible.
Nomura has been battling retinitis pigmentosa for over 40 years.
He currently leads a patient association.
Retinitis pigmentosa can make it difficult to see in the dark.
Other symptoms include a reduced field of vision and weakened eyesight.
It's like rolling up a piece of paper and looking through it.
It's very inconvenient.
I sometimes bump into telephone poles.
I remember feeling terrified that I might go blind someday.
Nomura has lost most of his eyesight.
He can only tell if it's light or dark.
To treat this challenging disease,
clinical research is underway on transplanting retinal cells made from other individuals' iPS cells.
The doctor leading this effort is Hirami Yasuhiko.
We transplant retinal tissue derived from iPS cells. We refer to it as a retinal sheet.
This is a retinal sheet.
First, iPS cells are turned into what resembles a three-dimensional retina.
Cells that can sense light and those that will mature into the retina are extracted from this 3D retina.
They are used to create a retinal sheet with a diameter of one millimeter.
During surgery, this sheet is transplanted into the patient's retina at the back of the eye using a syringe.
The retinal sheet is thought to act as a replacement for lost photoreceptor cells.
The sheet gradually starts communicating with nerve cells.
This is believed to lead to the eventual improvement of vision.
The transplanted retinal sheet contains light-sensitive cells.
They connect to some of the patient's remaining brain nerves.
That probably enables the detection of light and the transmission of signals to the brain.
As a result, the patient will be able to sense light.
The research team did experiments,
transplanting retinal sheets made from iPS cells into mice with retinitis pigmentosa.
They found that four of the 10 mice became able to sense light.
After eight years of animal testing, retinal sheet transplants were done on two patients -
one in 2020 and the other the following year.
This image shows a cross-section of a patient's retina.
Before the transplant, it had become thinner due to a reduction in photoreceptor cells.
After the transplant, the parts where the retinal sheet was inserted became thicker.
A year later, these areas remained stable, indicating that the sheets had become part of the retina.
In this surgery, only small parts of the retina were transplanted,
rather than the entire structure, for safety reasons.
We confirmed that the patients didn't have any severe side effects after their transplant.
I'm hoping to transplant bigger sheets that can cover a larger area of the retina.
Sheets that connect with patients' neurons more efficiently would also be beneficial.
I hope further studies will lead to such improvements in retinal sheets.
Then we might be able to observe improved vision in patients.
If I could see better, even a little, life would be less inconvenient for me.
I hope research will progress so that my vision will get better.
Japan is at the forefront of regenerative medicine.
Regenerative eye therapy using iPS cells is progressing toward practical use,
thanks to the dedication of doctors and also other researchers.
And we look forward to further developments,
both in Japan and also overseas, to benefit the many patients in need of treatment.
Today on tips for healthy living.
We're going to be covering juices which are really good for eyestrain, eye fatigue and overall body fatigue.
And we're joined by the lovely Akiko Furutani, who is a registered dietitian.
So, Dr. Akiko, what sort of juices are really good for eye fatigue?
We believe that when the body recovers from fatigue, eye fatigue also disappears.
Tomato juice contains lycopene.
You can absorb more lycopene by drinking tomato juice than by eating fresh tomatoes.
Lycopene is a nutrient found in tomatoes.
It's believed to help remove a source of fatigue called reactive oxygen species.
Cheese can help to boost lycopene absorption.
Lycopene is fat soluble.
Therefore, Furutani recommends having tomato juice with olive oil or dairy products to improve lycopene absorption.
Your body absorbs more lycopene in the morning than in the evening.
That's why morning is a good time to drink tomato juice.
Furutani is an expert in chrononutrition,
which focuses on studying when and what to eat to maximize health benefits.
We absorb various nutrients and build body components as part of metabolism.
How well the process works depends on the time of day.
Lycopene, for example, is best absorbed by the body in the morning.
In an experiment, a food maker had people consume lycopene in the morning, noon, and evening.
Blood tests showed the highest lycopene absorption rate in the morning.
Carrot juice is also recommended for fatigue.
Experts say beta-carotene, contained in carrots, can remove reactive oxygen species from the body.
Drink this in the evening.
Furutani says that because carrots are also rich in potassium and low in carbohydrates,
they can prevent high blood pressure and blood sugar to maintain restful sleep, helping with fatigue recovery.
Those who don't like carrot juice can try soup.
First, combine sliced onions and a teaspoon of powdered stock,
then microwave for three minutes at 600 watts.
Next, pour in 100 milliliters each of carrot juice and milk,
and microwave for one more minute at the same power.
Add salt and pepper to taste, and your carrot and onion soup is ready.
You can use soy or almond milk instead of regular milk if you prefer.
Another well-known food for fatigue recovery is lemon.
It's rich in vitamin C.
Lemon juice is believed to have different effects depending on when it's consumed.
Vitamins taken at night are very effective for fatigue recovery during sleep.
At nighttime, they help with fatigue. In the morning, they protect against UV stress.
If juicing is a hassle, I recommend this.
A fantastic idea.
Because I think everybody has ice cube makers at home. So that's a really good idea.
Unlike regular ice cubes, this won't dilute your drink, so you can enjoy it to the last drop.
Okay great.
The final recipe was created by Erica.
It's a tofu and pineapple juice that's very easy to make.
Just combine tofu, pineapple, honey and ice cubes, then puree them.
Please try it.
See what it tastes like.
It's delicious. It's tofu, but it doesn't taste like tofu. The honey adds a really nice touch.
Raw pineapple contains bromelain, an enzyme that breaks down proteins.
It makes the tofu's proteins easier to absorb. This juice is perfect for the morning.
Dr. Akiko, there were so many fantastic tips and really, really practical tips for people who are really busy.
Drinking these juices for a day won't be enough to get rid of fatigue.
First, try them for a week, then aim to make them a part of your daily routine.
So thank you so much.
Thank you.