Genomic Testing for Lung Cancer
The five-year survival rate for lung cancer is increasing. Tests can now identify gene mutations, enabling treatment with targeted drugs. We share the latest developments in lung cancer treatment.


Transcript
Join us as we explore Medical Frontiers!
Lung cancer claims more lives globally than any other form of cancer.
Fortunately, the 5-year survival rate for the disease is increasing steadily
thanks to advances in new cancer drugs and genetic testing.
Japanese doctors are conducting detailed testings on the characteristics of each patient's cancer-related genes.
This personalized approach not only enhances the effectiveness of treatment
but also helps to improve quality of life.
Today on the program, we will focus on the forefront of lung cancer treatment here in Japan.
Data shows the five-year survival rate for lung cancer patients in Japan
recently rose from 35.2 percent to 43.2 percent.
A notable improvement was also confirmed for stage 4 patients.
Almost 17 years have passed since Haga Miyuki was diagnosed with stage-four lung cancer.
The revelation came out of the blue.
I don't smoke, so I thought, "Why me?"
Lung cancer, typically associated with smoking, can also affect non-smokers.
Research in Japan shows that 75 percent of female lung cancer patients have never smoked.
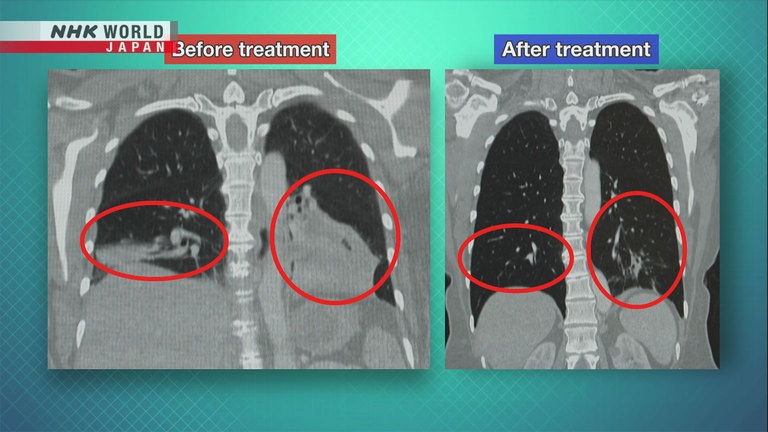
This CT image shows Haga's lungs at the time of diagnosis.
The white part at the bottom of the left lung, circled in red, is the cancer.
Measuring about 9 centimeters, it had spread to the right lung and other areas.
However, after undergoing several drug therapies, her tumor shrank.
Since then, it has remained in stable condition.
The key to her treatment was genomic testing of her tumor.
Kitasato University Hospital is using genomic testing to find drugs that are suited to each lung cancer patient.
The pathology department receives around 27,000 tissue samples annually
from patients suspected of having cancer or other diseases.
To test for lung cancer, a bronchoscope is inserted through the mouth or nose into the lungs to collect tissue samples.
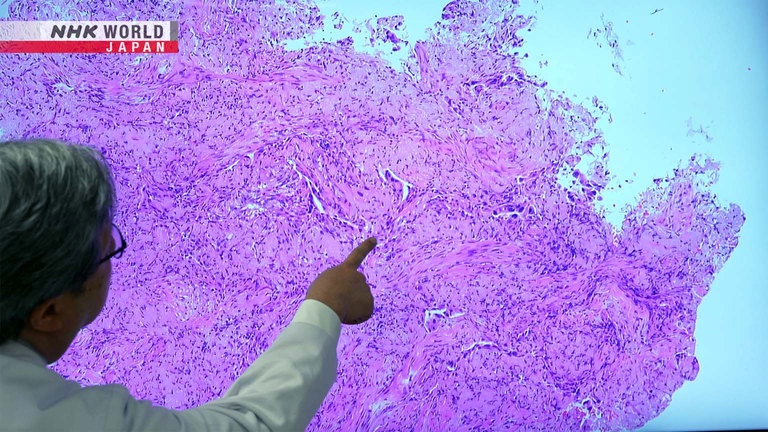
Yoshida Tsutomu has 25 years of experience in pathological diagnoses.
Most of the cells here are cancerous.
I would say about 60 to 70% of the cells
in this sample are cancer cells.
In the past, the pathological diagnosis team was responsible for checking samples with microscopes,
determining whether they were cancerous, and making a definitive diagnosis.
But it now also conducts genomic analyses of the cancer cells.
We've identified the driver gene as EGFR.
There are two methods of analysis depending on the amount of cancer cells.
The department aims to identify the cancer driver gene,
which plays a direct role in cancer development and progression.
We asked Sasaki Jiichiro, one of the experts who created guidelines for patients at the Japan Lung Cancer Society,
how identifying the cancer driver gene contributes to treatment.
We often tell our patients that there's
a gene that acts like the boss.
We can tackle cancer by defeating
this boss - the cancer driver gene.
When our cells multiply abnormally due to damage to the genes, we eventually get cancer.
Cancer driver genes act as "bosses" that instruct this cell growth.
When prompted, normal driver genes activate the switch that signals for cell growth.
However, mutations in these driver genes can permanently activate the switch, even without prompts,
sending continuous signals for cell growth.
As a result, the cells continue to multiply, leading to cancer.
What's interesting is that the cancer driver gene
is like the kingpin for the cancer.
Each lung cancer patient has
only 1 type of cancer driver gene.
Studies are being conducted to find ways of stopping cancer cell proliferation
by controlling cancer driver genes.
In 2004, researchers discovered that the EGFR mutation was directly linked to lung cancer development and growth.
Since then, many other cancer driver genes have been identified around the world.
What are the key benefits of knowing this specific genetic mutation?
It enables us to provide optimal treatment.
If we can identify the genetic mutation,
we can choose the best medication for it.
These medications are known as molecular targeted drugs.
So far, drugs targeting nine cancer driver genes have been developed.
About half of non-small cell lung cancers involve driver genes.
Patients are given drugs that target the identified gene.
Once targeted drugs enter cancer cells, they usually bind to proteins produced by the driver genes.
They turn off the switch that signals cell growth,
halting the proliferation of cancer cells and triggering cell death.
Conventional anticancer drugs attack both cancerous and healthy cells.
Meanwhile, molecular targeted drugs pinpoint cancer cells and are less burdensome on the body.
Doctors can control the side effects of targeted drugs more easily,
enabling patients to lead relatively normal lives.
However, targeted drugs cannot eliminate cancer.
Many patients need to take these drugs long-term.
I guess the side effects are a lot less than traditional chemotherapy.
The side effects of targeted drugs are
different from those of anticancer drugs.
They're milder, but they can be
challenging for some patients.
Side effects such as acne, cracked nails
and diarrhea may not be life-threatening.
But they can cause discomfort.
Therefore, it's crucial for us
to educate patients on self-care.
It's also important to provide guidance
on managing these side effects.
Haga, who was diagnosed with stage-four lung cancer, received chemotherapy,
then switched to targeted therapy.
The targeted therapy caused itchy skin and diarrhea, but she has found it far less taxing.
It was stress-free.
I didn't lose my appetite nor get nauseous.
It made my days brighter.
All I had to do was to take 1 tablet
a day, and I could live a normal life.
Genomic testing was not yet common when Haga began targeted therapy in 2008.
She started it without knowing which cancer driver gene she had.
To receive the treatment, you had to be
an Asian woman who had never smoked.
I was a perfect match,
and they suggested I try it out.
I was desperate, as my cancer was
in stage 4, and it was growing and worsening.
Excuse me.
Haga received genomic testing in 2023.
It revealed that she had the EGFR mutation.
The drug she had been taking happened to be effective against it.
After chemotherapy and molecular targeted therapy,
her tumor shrank and has hardly shown signs of regrowth.
This enabled partial removal of her left lung.
She is no longer taking medication.
There's no sign of a relapse,
but we'll continue to monitor it.
We might have to think about
what to do if it returns.
- Is there any drug I can take then?
- Yes.
Knowing which cancer driver gene is involved makes it easier to create a treatment plan.
Currently, there are five molecular targeted drugs for the EGFR mutation in Japan.
Thanks to national health insurance,
which covers part of the cost of genomic testing for lung cancer, survival rates have risen.
She's still alive and very healthy, living a very active life 17 years later, which is which is amazing.
How do you feel, though, that she's incredible to see 17 years later?
These 17 years have given us hope.
We know she has the EGFR mutation,
so we can give her other drugs if needed.
That gives us more hope.
However, half of non-small cell lung cancers,
do not have cancer driver genes for which molecular targeted drugs are available.
So then if no driver mutation is found, for example in a patient is got for example of I'm coming to you,
does that mean that I there's no tailored or effective treatment specifically for me?
Various drugs have been developed
to target certain driver gene mutations.
Many patients are disappointed when they
find they have none of these mutations.
But there are other suitable treatments for them.
We tell them that we can combine conventional
anticancer drugs to offer optimal care.
Cancer treatment using molecular targeted drugs involves another challenge, known as drug resistance.
Continued use of such drugs can cause new mutations to develop in the driver genes.
The drugs become less able to bind to their target, becoming ineffective.
Typically, this occurs after one or two years of taking the targeted drug.
The cancer cells resume proliferation, and patients are forced to switch to a new drug.
As this cycle repeats, patients eventually run out of treatment options.
Katayama Ryohei has been seeking solutions for patients who have developed drug resistance.
A bag of liquid arrived at his lab from an adjoining hospital.
Thank you.
This is freshly collected, very warm
pleural fluid sent from the pulmonologist.
In lung cancer, inflammation caused by the tumor can lead to a build-up of a large amount of fluid
in the space surrounding the lungs, called the pleural cavity.
When there's too much fluid, it can press against the lungs and heart,
and it must be removed using a needle.
This fluid contains numerous cancer cells, which appear as cloudy, white particles.
Katayama uses these fluid samples to research suitable drugs from among existing options
for patients with drug resistance.
A tumor that's about 1 cm in size usually
contains around 500 million to 1 billion cells.
The cancer is constantly undergoing
changes to produce cells that can survive.
That's its survival strategy.
Katayama is now focused on investigating drug resistance in lung cancer patients with the ALK fusion gene.
There are currently five molecular targeted drugs available in Japan for ALK-positive lung cancer.
However, after trying two or three drugs,
many patients develop powerful drug resistance that renders other drugs ineffective.
To tackle this challenge, Katayama extracted cancer cells from patients' chest fluid and cultured them.
They were placed in the wells on a microplate and exposed to numerous drugs,
including those for diseases other than lung cancer.
Three days later, the wells were inspected to identify those where the cancer cells had not increased.
Katayama ensured the drugs used in those wells were effective.
He then administered them to mice that had been implanted with human cancer cells.
These painstaking efforts bore fruit in 2021,
when Katayama's team found that a drug for acute leukemia was effective against ALK-positive lung cancer cases
where strong drug resistance had developed.
I couldn't help but say "Yes! Yes!"
I thought it was incredible.
Katayama experimented on four groups of mice.
One was not given any drug, the second was given the drug for acute leukemia
and each of the remaining two were given different targeted drugs for the ALK fusion gene.
The black line shows mice that didn't receive any drug; They died after around 10 days.
The red line shows mice given the leukemia drug.
Their tumors shrank and stayed small.
Katayama's focus was on the two groups given targeted drugs.
These drugs eventually stopped working, and the tumors started growing again.
But when switching to the leukemia drug 40 days later, the tumors in both groups shrank.
I was convinced of its efficacy as the tumors,
which had grown with conventional drugs, shrank.
The findings received international praise.
In 2024, a clinical trial using this acute leukemia drug for lung cancer patients
is scheduled at the University of Michigan in the United States.
I hope this therapy will prove
effective and not cause any harm.
I want it to allow patients to live
longer and better lives.
My aim is to see at least some types of
cancer, if not all, treatable with medication.
Do you have any specific advice or perhaps even a message for lung cancer patients?
Nowadays, undergoing various tests
and receiving optimal treatment has
greatly extended the time people
can continue their current lifestyles.
This increases their chances of
encountering the next breakthrough treatment.
So, I want patients to view their current
treatment as paving the way for the future.
However, it's not ideal if treatment
becomes the sole purpose of their lives.
It's crucial for people to find joy
in their daily lives as well.
Ultimately, I want to convey the message that
there's always hope for future treatments.
Kitasato University Hospital has what it calls a "cancer salon,"
where patients and their families can share their thoughts and concerns.
Among the participants is lung cancer patient Haga.
Although advancements in medicine have improved survival rates,
treatment continues as long as there is no cure.
Four women shared their approaches to dealing with cancer and what they're mindful of in their daily lives.
Tamaoki developed blood cancer in 2005, and later, colon cancer.
It spread to her liver, and she is undergoing treatment.
Mori is being treated for ovarian cancer.
And this patient has completed treatment for skin cancer and is currently under observation.
I feel energized after talking to them.
Indeed.
I always feel better after visiting the salon.
I went to the cancer salon in tears.
But everyone welcomed me with smiles and words
of encouragement like, "Let's hang in there."
It gave me the courage to have 2 more surgeries.
We understand each other.
I'm grateful I have fellow cancer patients
as friends. I can really talk to them.
That's what "cancer buddies" are for.
We can talk about cancer without holding back.
Once treatment starts, patients encounter various challenges,
such as side effects from medication and the lingering effects of surgery.
Haga learned how to cope with diarrhea, a side effect of her molecular targeted drug, to avoid giving up her interests.
I noticed that I get stomachaches
whenever I eat ramen.
It usually starts about 6 to 8 hours afterward.
Giving up my favorite food would be
too stressful, so I decided to keep enjoying it.
I know that I'll have to dash to
the bathroom 8 hours later, but it's worth it.
It doesn't stop you.
No way! It's my favorite food.
But you can be prepared if
you know what to expect later.
Exactly.
Patients often feel distressed during treatment.
But these women know how to uplift themselves during such moments.
I kept telling myself that one day,
I'd smile naturally again.
I kept believing that enjoyable things would
happen, making me laugh, just like before.
When I feel down, I talk to my late husband
at the Buddhist altar at home.
Expressing my emotions this way brings me comfort.
- You speak to the altar?
- Yes.
In living with cancer, these women share something important.
If I continue to enjoy life, my family
will think I had a good life when I die.
They might feel some regret, but I want
them to think I lived my life to the full.
I try to stay positive, no matter what.
I've decided to live joyfully.
It's not fun to live with a disease.
But I want to always be cheerful
and have a smile on my face.
I now feel that cancer isn't all that bad.
It has connected me with these people.
My goal is to maintain my current lifestyle
and travel with my friends.
I want to live cheerfully and without constraints.
I want to travel across Japan
to rediscover my home country.
I hope to make memories that will
keep me going for the rest of my life.
I want to treasure each day and continue smiling.
Even with cancer, you can certainly still live a full life.
And I strongly feel that advancements in medical care support patients,
giving them hope and courage to continue to lead full and active lives.
And I hope for a future where research progresses even further,
and personalized treatments tailored to each patient become the standard of care.