Special Episode: iPS Cell Research - Advancing into the Future
Prof. Jun Takahashi succeeded Nobel laureate Prof. Shinya Yamanaka as director of Kyoto University's CiRA. Find out the goals under the new leadership as we look at the latest research on iPS cells.
Transcript
In the 21st century, the field of medicine is undergoing dramatic changes with the discovery of iPS cells.
Kyoto University's Center for iPS Cell Research and Application, or CiRA,
is at the forefront of this world-class research.
Since its establishment in 2010,
CiRA had been led by Professor Shinya Yamanaka, the Nobel laureate who discovered iPS cells.
However, in 2022, the role of director was succeeded by Professor Jun Takahashi.
What are the goals and aspirations of CiRA under the new leadership?
Today, we get a chance to interview Professor Takahashi
to find out and also learn about CiRA's latest research and breakthroughs. Let's go.
- Hello. Good afternoon.
- Hi. Good afternoon.
Thank you for having us today.
- Yeah, Welcome to CiRA.
- Thank you.
- Please come in.
- Thank you.
Inside his office, we were greeted by a Japanese samurai armor.
You have a big Japanese samurai armor. Why do you have it in the office?
Yeah, yeah. This is to inspire me and my colleagues.
In which way does it inspire you?
Yeah, yeah. So it reminds me of the fighting spirit and the spirit of never give up.
And also, the partition here, it looks quite precious. Is it a famous one?
Ah, yes, yes, this is painted in the Edo era. I love elephants.
Because the elephant is very wise and powerful, but gentle.
I want to begin by talking about Professor Yamanaka, the former director of the institute.
He not only discovered iPS cells, but also became a Nobel Prize laureate,
leading the institution with a charismatic nature.
He was also very active in speaking out on various social issues, including COVID-19.
How do you feel about succeeding such a great leadership?
Of course, there is pressure.
But Yamanaka Sensei is Yamanaka Sensei, and I am me.
So, I can only do things my way.
And I was one of the founders of this institute, and I was involved from the beginning.
I mean, from writing the blueprint of this building.
Our role is to lead the world in both basic research and the clinical transplantation of iPS cells.
So, as you may know, now there are 14 clinical trials ongoing in Japan and using iPS cells.
But for the better or safer and the more efficient treatment,
we need to improve the quality of iPS cells.
Now, let's take a look at the research of Associate Professor Yasuhiro Takashima,
that is expanding the possibilities of iPS cells!
Working in front of the computer is Associate Professor Yasuhiro Takashima.
He's not writing a paper, but rather, he's posting something on his Instagram.
This is a video of Takashima in his beloved hometown in Himeji,
helping to carry a portable shrine on his shoulder.
He has been participating in the festival almost every year.
and consider joining CiRA or my group.
I use Instagram in hopes that
young people can learn more about me
and consider joining CiRA or my group.
Takashima's studies have revolutionized iPS cell research.
It all unfolded during his time at the University of Cambridge in the UK.
It is said that iPS cells, which are derived from blood cells,
are all-purpose cells that can turn into any type of cell.
Strictly speaking, however, this is not entirely true.
When a sperm enters a woman's body and joins an egg, it fertilizes it.
At this point, the roles of the cells are not yet determined.
The fertilized egg eventually becomes an embryo and attaches to the lining of the uterus.
This is known as implantation.
Once implanted, the cells differentiate into various organs and eventually form into a fetus.
iPS cells were planned to reverse time and return the cells to the state before differentiation began.
However, in reality, the cells had already begun to differentiate.
Our bodies are formed based on
the genetic memories of both parents.
That memory is reset
during the formation of epiblast,
just before implantation.
Our entire body forms from this epiblast.
Although we try to make iPS cells
mimic the fertilized egg,
human iPS cells don't seem to
fully regress to that stage.
Some iPS cells may differentiate
into heart cells, but not into nerve cells.
On the other hand, it's impossible that
a fertilized egg within the human body
can't differentiate into certain cells.
That's why I've focused on bringing
human iPS cells closer to fertilized eggs.
iPS cells of mice have been invaluable,
since they behave more like fertilized eggs.
Takashima realized that the clusters of iPS cells derived from mice were small and in a state
that was similar to the cells before implantation.
So, why not create cells similar to those of mice?
After much trial and error, Takashima and his team discovered a factor
that enabled iPS cells of mice to become an undifferentiated state of just before implantation.
They added this factor to human iPS cells and cultured them.
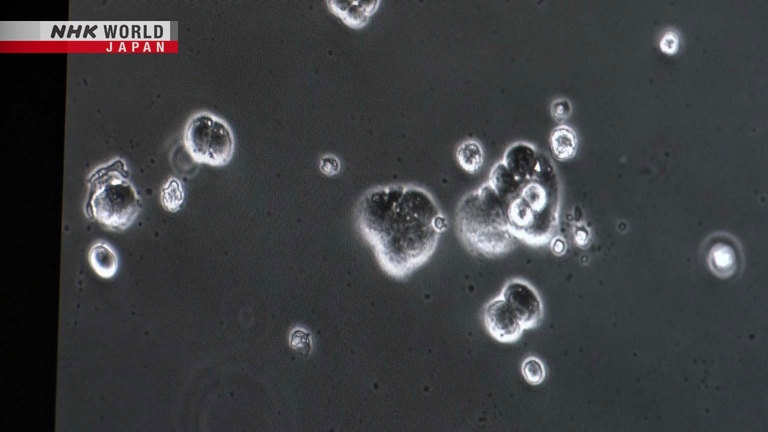
Let's take a look at the cultured cells under a microscope after 28 days.
They have been named naïve human iPS cells.
Each of these colonies contains
a few dozen to a hundred cells.
When seen at this scale,
conventional iPS cells are larger and flatter.
Naïve iPS cells are smaller
and bulge out more.
When they are close to fertilized eggs,
each cell loses polarity and becomes spherical.
When compared at nearly the same scale,
we can see that the clusters of naïve iPS cells are much smaller than the conventional iPS cells.
When we first created naïve iPS cells,
I was relieved and thrilled.
I thought we finally did it.
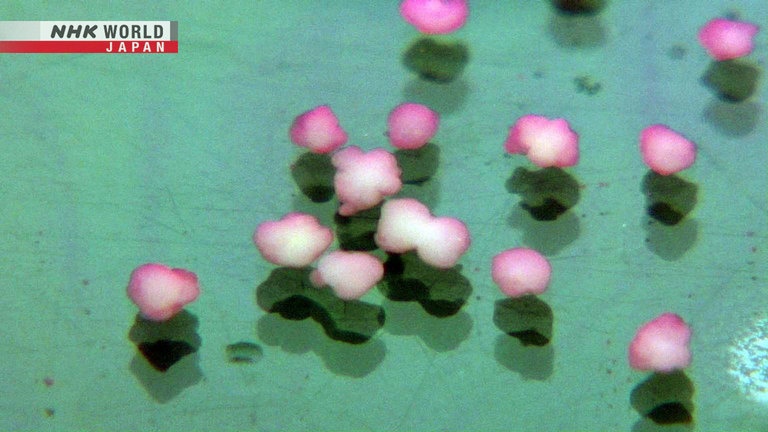
Using naïve iPS cells, Takashima and his team also succeeded in creating placental cells,
which could not be produced with conventional iPS cells.
The placenta plays a crucial role in supplying nutrients from the mother to the fetus.
These are placental cells made from naïve iPS cells.
Takashima has set many goals.
One of them is to pave the way for treating illnesses during pregnancy.
Expecting mothers often face illnesses
which have no clear causes.
This is partly due to
the limited studies of the cells.
In worst cases, they have no treatment option
but to terminate the pregnancy.
In less severe cases,
conditions are managed with rest and IV.
Naïve iPS cells can help us better understand
the disease and move forward.
Takashima is also working on creating a model of an embryo before it becomes a fetus.
His second goal is to shed light on the process of human birth.
What an embryo model can tell us
in the near future
is how it implants in the uterus.
We can also understand the way
our body's fate is determined.
Further in the future, we want to create
iPS cells that can be used on patients.
We've succeeded in creating what seemed like
liver cells or heart muscle cells
by inducing differentiation from iPS cells.
However, the early development
still remains a black box.
Understanding the mechanism will lead to
induction methods that are physiologically similar.
Currently, organs like the liver
that contain blood vessels and nerves
cannot be derived from iPS cells alone.
Creating embryo models can help us make
physiologically accurate mini-organs.
Up until now, not all cultured iPS cells could be used.
Naïve iPS cells have a high rate of producing quality cells.
Takashima's third goal is to make iPS cells more affordable and widely available.
Cost reduction is very important.
It costs tens of millions of yen
to make iPS cells.
To make what Yamanaka sensei
refers to as "My iPS cells,"
we must make it more accessible,
and cost reduction is essential.
Dr. Takahashi hopes to have hospitals
produce iPS cells, instead of factories.
Patients get a blood test and can have
iPS cells made onsite for immediate use.
Only then can iPS cells become accessible.
This dream resonates deeply with me.
Takashima still faces challenges with naïve iPS cells, such as having a limited culture period.
He and his team are working to overcome each challenge to realize their dreams.
It already smells so good.
So wait several seconds for steam.
- I love it when it blows up like.
- Yeah, yeah, yeah. It should be.
- What got you started?
- I don't remember.
Yeah. But I don't have, you know, time to go out for lunch.
So I always have lunch here.
And... yeah. And enjoy coffee.
Thank you very much! It smells wonderful.
I have chocolate here.
And it tastes so good.
I love deep roast. So this is excellent.
What are your thoughts on Dr. Takashima's research?
We need to improve the quality of iPS cells.
And there are three points.
One is safety.
So, if his research will be successful, the safety of the iPS cells increase.
The possibility of the changing to the cancer cells, it can be lowered.
And also, the current iPS cells, if we make for example 10 iPS cell lines, among them,
about two or three cells can be used for the clinical treatment.
But by Takashima Sensei's research, nine or 10, almost all the cells can be used for the clinical treatment.
- That's amazing.
- Yes.
And the third one is stability for the differentiation.
For the treatment, we need to make neural cells or cardiac cells from the iPS cells.
But this process is not stable.
But by Takashima Sensei's research,
these cells, neural cells or cardiac cells can be made very stably.
So, in what other field of research do you think will be important in the future?
Of course, all the researches are important, but in terms of the point,
which is very close to the clinical application,
there is immunotherapy by using iPS cells to treat cancers.
That is one big goldfish.
It lives in a tank inside Professor Shin Kaneko's office.
When I approach,
it knows it's time to eat.
It was only 4 cm at first.
Now, the fish is around 10 years old.
It's big and healthy.
It's calming to watch it swim around.
The immune cells Kaneko created from iPS cells are about to revolutionize cancer treatment.
Human beings have immune cells that attack bacteria, viruses, and even cancer cells in order to protect the body.
Research has been underway worldwide aimed at strengthening immunity to treat cancer.
However, they face numerous challenges.
I believe there are 3 factors
to enhance immunity.
First, the immune cells must accurately
recognize and target cancer cells.
Second, they must be young, healthy and active.
Finally, there must be a sufficient number
for fighting cancer.
When I was exploring different methods,
I came upon Dr. Yamanaka's report on
the successful generation of human iPS cells.
I immediately saw its potential in this approach.
iPS cells can produce young, newborn cells.
And these cells can proliferate indefinitely.
This is a type of immune cell known as Natural Killer cell, or NK cell.
They attack when cancer cells or viruses are nearby.
To enhance the capability of detecting cancer cells,
Kaneko and his team added special proteins to iPS cells.
Next, factors that convert iPS cells into NK cells are added and cultured.
They have successfully produced a large quantity of NK cells.
Moreover, they exhibit stronger attacking capabilities against cancer compared to regular NK cells.
This is the National Cancer Center Hospital East.
Here, clinical trials have been underway since 2021
in which NK cells developed by Kaneko and his team are transplanted into patients with ovarian cancer.
NK cells that are made from iPS cells are immune cells that have relatively few side effects even when transplanted.
If the trial proves its effectiveness and confirms its safety,
it will be a big advancement in immunotherapy for cancer patients.
In terms of safety, it's proceeding smoothly
without any major side effects.
It can be readily accessible to many people.
This is a major advantage compared to
the conventional CAR-T immunotherapy.
It's a promising new treatment.
By the way, Dr., I'm a little bit curious. What is behind the partition?
- This is secret... secret place.
- A secret place?
- Mm-hm.
- What do you mean?
- So no one ever seen over the partition.
- Really?
That was amazing!
- Oh, wow! So that was your secret.
- Thank you very much.
But what does piano mean to you then?
- Just fun.
- Okay.
- So it... it helps you give... feel fun in your life?
- Yeah, and relax.
And iPS cell research is also very expensive, right?
What are your plans regarding the financial aspects of CiRA?
Yeah, as you mentioned, donation is very important.
And a good thing is a lot of people give us donation.
And it is very helpful to advance our research
and also to prepare the research environment for the young researchers.
Are there any other efforts that are underway?
Yes. Professor Kaneko created his own venture company
and succeeded to raise funds and advance his research.
The startup founded by Professor Kaneko is located on the campus of Kyoto University, just a few minutes' walk from CiRA.
They are also based in the US, aimed at proceeding with clinical trials there.
The partnership is invaluable for helping
our research findings reach patients.
With Kyoto University Hospital nearby and
the cell manufacturing facility next to our lab,
everything is packaged together
including basic research,
clinical development and application.
Kaneko's next goal with the startup is transplanting another type of immune cell called killer T cells.
Killer T cells are powerful immune cells with the remarkable ability to clearly recognize targets anywhere in the body.
They are essentially the ultimate weapon of the immune system.
Kaneko and his team have developed enhanced killer T cells from iPS cells,
boosting their attacking capabilities.
Moreover, they have incorporated receptors that recognize specific cancers in advance,
maximizing their effectiveness.
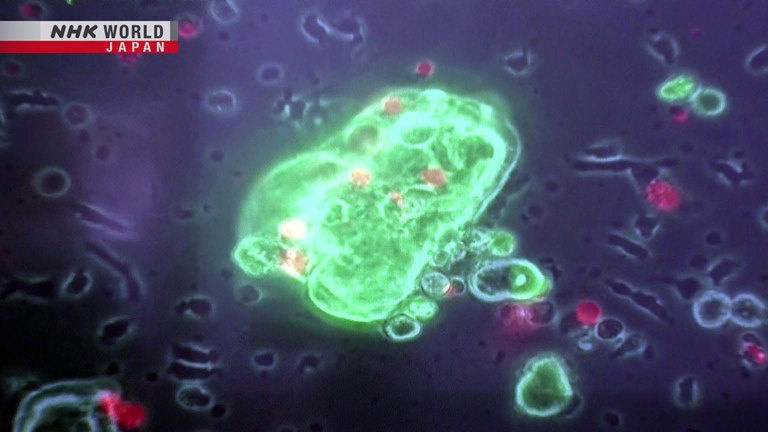
The killer T cells created by Kaneko are mixed into cultures containing cancer cells.
The glowing green cells are
clusters of colon cancer cells.
There are dark cells moving actively,
penetrating into the cancer.
Those are killer T cells.
Can you see them turning red?
When cancer cells turn red, it indicates cell death.
Each cell in the cluster of the colon cancer
is undergoing attack by the killer T cells.
This shows how regenerated killer T cells
have the ability to destroy the clusters.
We've received funding and are in the
process of moving towards clinical trials.
If all goes well, we'll reach clinical trials
in the not-too-distant future.
Science has two directions.
One is for the fundamental, or basic research to find the way how this world or universe works.
Another one is for more application research, to make this world or society better.
And as a medical doctor or physician, I would like to use my research or my work for the treatment of patients.
So, you yourself take it one step, two step further.
Yeah.
Will you be continuing your own research while taking on the intense workload of being the director?
Yes, of course.
Our motto is to build a brain.
So now, we are trying to make a brain organoid, the cell aggregation of the neural cells from iPS cells.
Our concept is to make a brain circuit by transplanting the neural cells.
And the first target is Parkinson's disease.
And now we are trying to make a treatment for the stroke patients.
Yes, that's very important research.
And finally, how do you envision the future of CiRA 10 years or 20 years from now?
It's a great question.
- It's a big picture.
- Yeah, yeah.
Because of the birth of iPS cells, now we are able to cure ourselves by using our own cells.
And also, the gene editing or gene delivery technologies are greatly advanced these days.
And these three technologies are awarded for the Nobel Prize.
So, I am very excited.
So, these three, the combination of these three technologies,
iPS cells, gene editing and gene delivery, will make our world much, much better.
- I can't wait.
- Yeah.
And the time when we can cure ourselves by our own cells will come.
I'm looking forward to that time.
- That's going to be a real game changer.
- Yeah.
Thank you so much for your time today, Dr. Takahashi.
Yeah, sure. Thank you very much.
Under the new leadership of Director Takahashi,
researchers at CiRA in Kyoto are dedicated to saving people around the world.