With coronavirus wards filling up around the country, many people are dying while waiting to be admitted to hospital. A state of emergency that is in effect across six prefectures aims to ease the strain on medical services.
Dementia a factor in infection spread
One of the biggest cluster infections has broken out at the Sunnyhill care facility in the city of Kobe. As of May 7, the facility had recorded 133 infections among its residents, with 25 deaths.
A staff member who spoke to NHK on condition of anonymity says the virus is spreading rapidly because many residents suffer from dementia.
"We are always asking residents to wear masks, but they usually take them off immediately," says the care worker. "Once an outbreak occurs, there is no way to contain it. That's why such a huge cluster has broken out here."
Medical resources in the area are stretched to breaking point and Sunnyhill doctors have been asked to care for infected residents at their own facility. As the condition of patients worsened, staff tried to get them admitted to hospitals—only to be rebuffed, in some cases because of a lack of available beds.
"We were making repeated calls to emergency services, but there was no facility that could accept the patients," recounts the staffer. "It's really frustrating that it's beyond our power."
He wants the tragedy to help younger people understand how frightening the virus can be: "Your grandfather or grandmother might die because of your infection."
Virus slips through PCR tests
Another cluster infection broke out at a nursing home in Osaka despite strict preventative measures. The Joto care facility had been refusing all visitors, including family members of residents – and staff were being tested two or three times a month.
Yet nine people, including workers and residents, were infected last month. Two of the residents died after being hospitalized.
Joto director Nakajima Motomi says she realized that infections could occur even when PCR tests are regularly conducted: "Some people were infected before anyone tested positive."
Associate Professor Takano Tatsuaki of Toyo University is an expert in nursing home management. He says the situation needs urgent attention.
"The prioritized vaccination of residents, as well as care givers and staff, should be done quickly," he says. "This will prevent cluster outbreaks and reduce the risk of staff members bringing in the virus from outside."
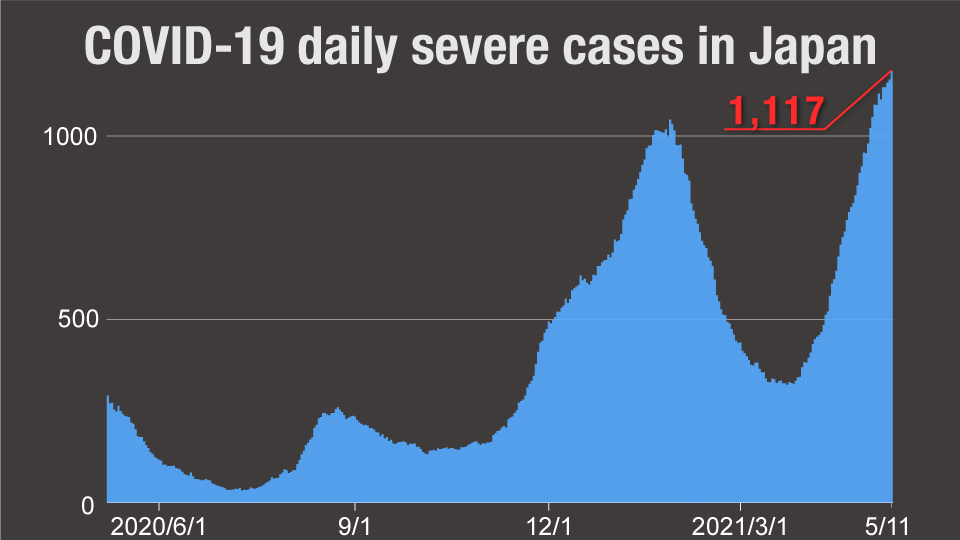
Japan's vaccine rollout has been particularly slow. In the meantime, the number of seriously ill COVID-19 patients in the country is hitting an all-time high. According to the Health Ministry, there were 1,177 such patients on May11.
Prime Minister Suga Yoshihide announced last week that the state of emergency intended to contain the virus is extended until the end of May. The area it covers has been expanded to include two more prefectures, bringing the total to six.
Omi Shigeru, the head of the central government's expert panel on the coronavirus, says the key focus is to reduce the strain on medical facilities. He maintains that is more important than tracking the number of infections.
He cautions the Suga administration against hasty decisions on the easing of restrictions. "The government should be more careful than ever when it decides to lift the current state of emergency," Omi says.



