Visualizing Tiny Blood Vessels in 3D
A new technology can capture clear images of tiny blood vessels using light and ultrasound. This will enable better treatments, such as reconstructive surgery for patients who have had a part of their head, neck or breast removed due to cancer. Doctors can safely cut and transplant skin flaps containing blood vessels from a different area of the body, decreasing the burden on patients. The technology can also visualize transparent, thin lymph vessels, and improve the treatment of lymphedema.



Transcript
Join us as we explore Medical Frontiers!
Our bodies are filled with a vast network of tiny blood vessels.
Japanese researchers have developed the world's first technology that captures three-dimensional, high-definition images of them.
This footage is of a new diagnostic imaging technology that uses light and ultrasonic waves.
It was developed jointly by number of companies and academia in a government project.
The technology is a potential game changer not only in the diagnostic but also in prevention and treatment of diseases.
A startup is playing a leading role in putting this diagnostics imaging technology into practical use.
Mr. Yagi, it's such a great pleasure to meet you.
Takayuki Yagi leads the development project.
There are only four devices that can capture such images in Japan.
So this is it.
Yes.
The technology, called photoacoustic 3D imaging, captures images of blood vessels using light and sound.
To produce such images, the target area of the body is placed on a window measuring 18 by 29 centimeters.
- Can I try it?
- Yes.
So basically, for example, if you were going to look at my blood vessels, my blood,
you would put your hand like this?
So there's some water on it know is that water?
Yes. Sounds from the body need to be
conveyed to the sensors.
The human body is mostly water.
Having water here makes it easier for
the sound to travel and reach the sensors.
This technology visualizes blood vessels by causing the body to emit sound.
First, near infrared light, which is harmless to humans,
is directed at the target area through the window.
The red blood cells absorb light energy and expand.
When this happens, the red blood cells produce weak ultrasonic waves,
which travel through the water.
The waves are captured by 512 sensors arranged in a dome-like shape beneath the window.
The location of the blood vessels is determined by the time it takes for the waves to reach the sensors.
This enables the creation of three-dimensional images.
Yagi demonstrates how it works using his hand.
Shall we start?
This is real-time footage of
the blood vessels in his hand.
Our device creates 3D images.
We can show the depths using different colors.
Oh my gosh.
The detail is amazing!
The device can show the depth of each blood vessel using different colors.
Here, blood vessels close to the skin's surface are shown in blue while those deeper inside appear red.
The scan is completed in a few minutes.
Because the image is three-dimensional, it's possible to see the relative positions of the blood vessels and their overlap.
The device can also show live footage providing a detailed look at the flow of blood and the movements of the vessels.
It can show blood vessels down to
0.2 millimeters in diameter.
Is it about the width of a hair?
A hair from a Japanese person is
around 0.08 mm wide, so it's about twice that.
That's incredible.
This is an image of blood vessels taken with a CT scan.
Compared with this, the difference in detail is clear.
When you first saw that very first image of the photoacoustic 3D image,
I mean, what did you think and how did you feel?
I was totally surprised.
The clarity was astonishing.
So why then did you decide to focus all of your energy on this photoacoustic technology on blood vessels?
Of all the things inside the body, the blood
tends to emit sounds most in response to light.
This is why we focused on it from the beginning.
Conventional technologies require
a contrast agent.
When CT scans are used to check blood vessels,
patients will be exposed to radiation.
Photoacoustic 3D imaging doesn't involve
radiation exposure nor a contrast agent.
It can be used on anyone. That's a big plus.
Blood vessels may not be a major area of medicine,
but they're associated with many diseases.
A clinical trial is underway at the plastic surgery department of a university hospital in Kyoto
to apply photoacoustic imaging to medical examinations.
Detecting the location of minor vessels could make reconstructive surgery safer and less taxing on patients.
The trial targets such surgeries for patients who have had parts of their body removed
due to cancer in the head, neck or breast.
Skin flaps from the thigh or abdomen are transplanted to the affected area.
This patient will have reconstructive surgery on her left breast using a skin flap from her abdomen.
Five days before the surgery, doctors used photoacoustic imaging
to check the blood vessels in her abdomen.
The most important thing in the surgery is to take skin flaps containing vital blood vessels.
Blood vessels branch out and spread.
The flap will become necrotic if the vessels that branch out are severed.
Susumu Saito heads the research team.
He believes photoacoustic imaging can benefit reconstructive surgery.
It's crucial that we grasp how and in which direction
the vessels spread, and their thickness and length.
Conventionally, doctors have relied mainly on ultrasound scans to confirm the distribution and length of blood vessels.
However, they have limitations.
I'd swing the probe to predict the precise location,
using my knowledge and experience.
But it was not easy, even for me.
Photoacoustic imaging provides crucial information that conventional technologies cannot offer.
This is unbelievably clear.
- Incredible!
- It's way beyond my expectations.
The image maps the network of
blood vessels, like leaf venation.
It enables us to predict how far
the vessels spread before surgery.
The map of blood vessels is printed on a clear film,
based on the images captured through photoacoustic imaging.
Blood vessels close to the skin are shown in blue; those located deeper are in green.
For the breast reconstruction surgery, a skin flap was taken from her abdomen using the map.
The surgeon trimmed the blood vessels and fat in the flap and transplanted it to the affected area.
A large skin flap is preferable for breast cancer,
but that's not the case with head and neck cancer.
Defects in the head or the neck are smaller and thinner than those in a breast.
When a skin flap is taken so as not to damage the branched blood vessels,
it ends up being larger than the defect.
Multiple surgeries must be conducted to minimize it to match the defect.
Photoacoustic imaging can provide details on the spread of blood vessels,
enabling surgeons to prepare small, thin skin flaps.
We can prepare an extremely thin skin flap.
We will be able to produce a result
satisfactory to the patient with a single surgery.
Undergoing surgery multiple times puts
a large burden on cancer survivors.
It also delays their return to the community.
If we can reduce the number of surgeries,
patients would benefit hugely.
The principle of photoacoustic imaging was discovered in 1880 by Alexander Graham Bell.
Bell found that light can be converted into sound.
He invented the world's first wireless communication device, called a photophone.
Studies began in earnest around the year 2000 to apply this principle to medicine.
In Japan, Kyoto University and a major precision equipment maker launched a joint research project in 2006.
Yagi was the head engineer from the firm.
Technologies such as CT and MRI
were developed in the 1970s.
There has been no new imaging technology since then.
We wanted to produce a new field
using a new technology.
The study led by Yagi was chosen in 2014 for the government's program to promote innovative technology.
It received funds of nearly 25 million dollars, and grew into a major project involving 16 companies and universities.
Now, Yagi is running a company which develops and promotes photoacoustic imaging equipment.
Their product is close to practical use.
What's most important is to have a clear picture
of what we want to achieve 5 to 10 years from now.
Academia, industry and government
worked together toward shared goals.
This is what helped put us
at the door to success.
- So you put the hand for the door and you see the door opened.
- Yes, we're waiting for the door to open.
Photoacoustic 3D imaging can visualize not only blood vessels, but also lymphatic vessels.
In this footage, the lymph vessels appear yellow, and the veins, blue.
Lymph vessels are transparent and less than one millimeter wide.
They are closely associated with blood vessels.
Blood travels from the heart to the rest of the body via the arteries delivering nutrients and oxygen.
It then returns to the heart via the veins while collecting carbon dioxide and waste.
The lymph vessels pick up the waste that is not collected by the veins.
They merge with the veins before the heart.
When the lymph vessels are blocked, lymphatic fluid builds up,
causing swelling in part of the body, a condition called lymphedema.
A clinical study is underway at a university hospital in Tokyo to use photoacoustic imaging to treat lymphedema.
Kazuo Kishi, who heads the research team, saw photoacoustic images of lymph vessels for the first time in 2017.
I was utterly shocked.
I could see the lymph vessels and veins
in 3D from various angles. It was amazing.
Is it difficult to capture images of lymph vessels?
Yes, it's difficult because they're transparent.
We've always wanted three-dimensional
data on them before surgery.
But that has not been available until now.
Ok, turn around.
This patient in her 70's developed lymphedema after undergoing surgery for endometrial cancer around 10 years ago.
Her symptoms are especially severe in her right leg.
Cancer cells tend to spread via the lymph nodes, which filter lymph fluid.
The nodes are often removed during cancer treatment to prevent the spread of the cancer.
This stagnates lymph flow, causing lymphedema.
To alleviate swelling, surgery is conducted to connect the lymph vessels
which are blocked to nearby veins with the aim of improving lymphatic flow.
We'll check your lymph vessels.
She has a test before surgery to check the location of the lymph vessels.
The test requires the subcutaneous administration of a contrast agent which reacts to light.
With the conventional method, near infrared light is directed at the site.
The lymphatic fluid glows in response.
The doctor uses this as a guide to locate the lymph vessels,
and marks the likely locations with a red marker.
But the lymph that has drained out also glows, making it difficult to detect the accurate locations of the lymph vessels.
The team runs a photoacoustic scan, which also requires a contrast agent, for a comparison.
Put the sole of your foot here. Good.
Here's a lymph vessel.
The photoacoustic image clearly shows the outline of the vessels and how they spread.
The difference is obvious when it's compared with the images captured using the conventional method.
Photoacoustic imaging can also show veins, which appear in blue, together with lymph vessels.
Photoacoustic images show veins and
lymph vessels at the same time.
It's a big advantage because it enables us to see
where they run and where they cross.
2 days later, it's time for the woman's surgery.
We'll work on 6 lymph vessels.
As you can see here, 2 of them are in the thigh.
The conventional scan fails to detect the two vessels in the thigh.
We can't tell if the image is accurate
until we cut open the site.
But we've seen the vessels in
the photoacoustic images, so we're prepared.
That's not possible with conventional scans.
They time surgeries to end in five hours or less to minimize the burden on the patient.
Two surgeons work together to make as many connections as possible.
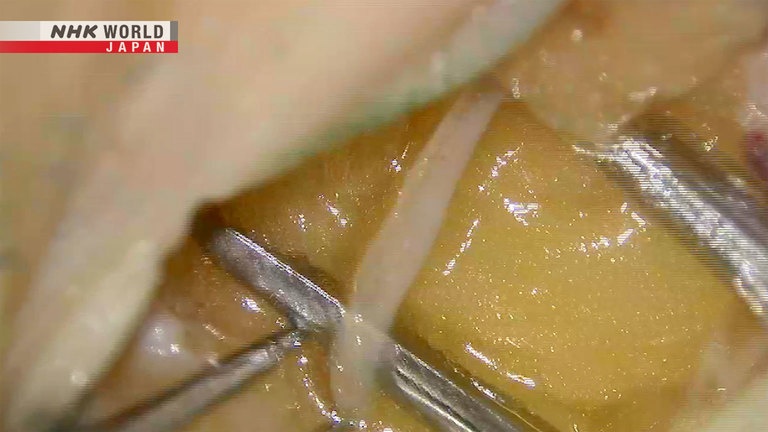
One of them starts working on a lymph vessel near the right ankle.
The transparent band is a lymph vessel.
The red one in the upper left is a vein.
The lymph vessel is 0.5 millimeters wide, while the vein is 0.9 millimeters.
Connecting them requires advanced skill.
It takes the surgeons an hour to stitch them together.
Fluid is flowing smoothly in the vessel and
the vein that have been connected.
Lymph fluid, which appears white, is flowing into the vein.
There must be something deep down.
They look for the lymph vessels in the thigh that appear only in the photoacoustic images.
It's difficult to locate the transparent lymph vessels in a thigh, where there is a lot of fat.
This one is good.
It's perfect.
Are they the ones we saw in
the photoacoustic images?
Highly likely. The thick one
and the one deep inside.
It's great we've got one this thick.
Thick vessels are easier to connect and expected to make major improvements in lymph flow.
Thank you!
The surgery is over after making seven connections, one more than planned.
The swelling in the patient's legs begin subsiding five days after the surgery.
Up until now, the effects of surgery could only be confirmed through changes in appearance.
But photoacoustic 3D imaging can visualize the flow of lymphatic fluid after surgery.
It shows the fluid flowing from a lymph vessel, which appears yellow,
into the connected vein, which looks blue.
There was no way to confirm whether they
remain connected after surgery.
Photoacoustic imaging can improve surgeries.
We've relied on our experiences when
determining where to connect and at what depth.
That's why we try to make
as many connections as possible.
But if we can make proper evaluations, we could
reduce the number of connections to a minimum.
That would make a big difference.
So what are some of the shortcomings then of the photoacoustic technology?
Currently, it can reach a maximum depth
of only 2 to 3 centimeters.
Another issue is the price.
The device will costs nearly one million dollars.
For the cost to decrease, the technology must be applied to more areas and become widespread.
Yagi has high hopes it will be used for the early detection of cancer.
This is a photoacoustic image of small blood vessels around a cancerous tumor in breast, colored in red.
Cancers grow their own blood vessels from a very early stage to get the nutrients they need.
Yagi believes that an accumulation of data on blood vessels unique to cancer could help with early detection.
Currently, needle biopsies using microscopes
are done to determine if cancer is proliferative.
The method uses a needle to extract tissue.
One of our major goals is to be able to
examine cancer without such procedures.
I hope the door opens very very soon as you show well.
Thank you so much for your time today.
Thank you.
Today on the program, we'll be learning some simple, easy acupressure points for self-care.
And today we are joined by the lovely acupuncturist, Dr. Mayumi.
- It's nice to see you again, Mayumi.
- It's good to see you too.
Today, we will introduce acupressure points to ease swelling and pain in the lower body, and frequent urination.
The first one is recommended for people with leg swelling.
Massage firmly in a circular motion
to increase circulation.
So then you're actually going in a circle with this one aren't you.
Yes. This helps move the muscles in your
calf, so it's very effective for swelling.
That's so interesting.
The second point is effective for knee pain.
It helps to improve blood circulation in the lower body and alleviate pain.
Use your thumb to apply pressure
in a circular motion.
It's painful.
This is also good for swelling.
Various massage tools are sold in Japan for about one dollar.
They include a ball that can stimulate acupoints in the hands,
and a massager for tight back muscles.
Oh, this one's great.
So this one's only a dollar, a hundred yen?
That's right.
That's amazing, because some of the spots are really, really difficult to reach yourself.
This wooden stick is also about one dollar.
It's perfect for pressing acupoints.
This is almost like a little drumsticks for a child.
Use the stick to press the acupoint to treat frequent urination,
located four fingers' width from the center of the inner ankle.
Oh Yeah. It's painful.
Press the point gently like this.
You may want to just rub it.
This is an excellent item as it can
press the point accurately.
And it's interesting you can use both side.
An acupoint for menstrual pain and menopausal symptoms is located another four fingers' width along the same line.
Yanamoto recommends gently tracing the line between the two acupoints.
You can also use the back end of a pen
or anything that has a similar shape.
There are a plenty of such items.
I think there's so many wonderful practical points that we can use.
So thank you so much for your time today.
Thank you.